It has come to my attention that the RCR offers almost no warning to international candidates whether they have, or do not have, a sitting for the FRCR final examination. This is clearly unfair and imposes candidates great costs for international travel at short notice. Unfortunately, for international registants for the Vlahos Grayscale course please note that it is not possible to offer a refund based on not obtaining an offer of examination from the Royal College of Radiologists. This is because the timeline does not permit filling the emptied space on such short notice. In a course designed for such a small group this has a significant impact on the financial viability of the course. The cancellation policy offers partial refunds for extenuating personal circumstances (other than RCR examination entry related), considered on a person by person basis. For more details please see updated cancellation policy on the registration and payment pages.
|
Places still available for Sep 5/6 and 12/13 courses.
It has come to my attention that the RCR offers almost no warning to international candidates whether they have, or do not have, a sitting for the FRCR final examination. This is clearly unfair and imposes candidates great costs for international travel at short notice. Unfortunately, for international registants for the Vlahos Grayscale course please note that it is not possible to offer a refund based on not obtaining an offer of examination from the Royal College of Radiologists. This is because the timeline does not permit filling the emptied space on such short notice. In a course designed for such a small group this has a significant impact on the financial viability of the course. The cancellation policy offers partial refunds for extenuating personal circumstances (other than RCR examination entry related), considered on a person by person basis. For more details please see updated cancellation policy on the registration and payment pages.
0 Comments
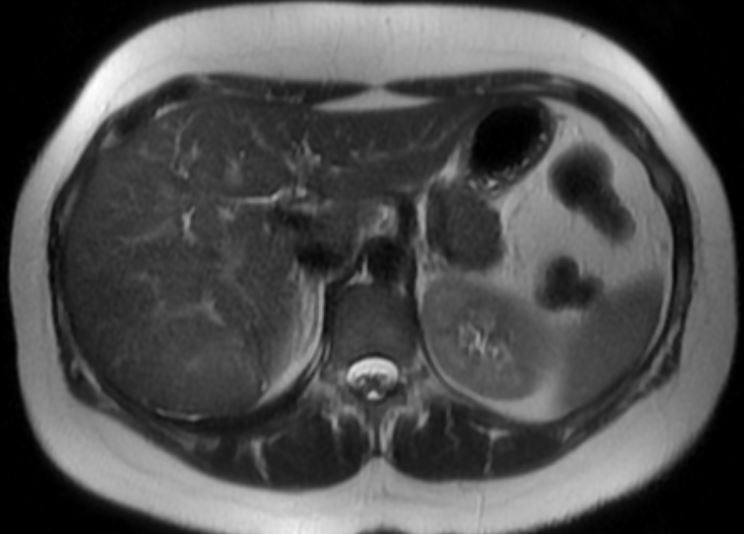
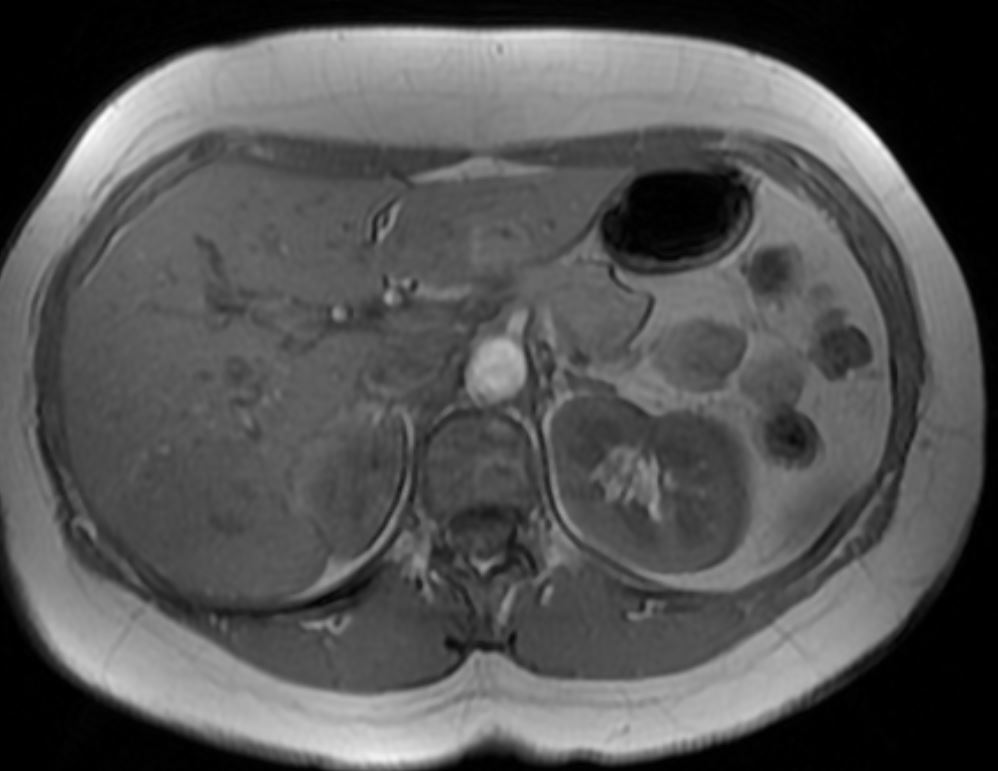
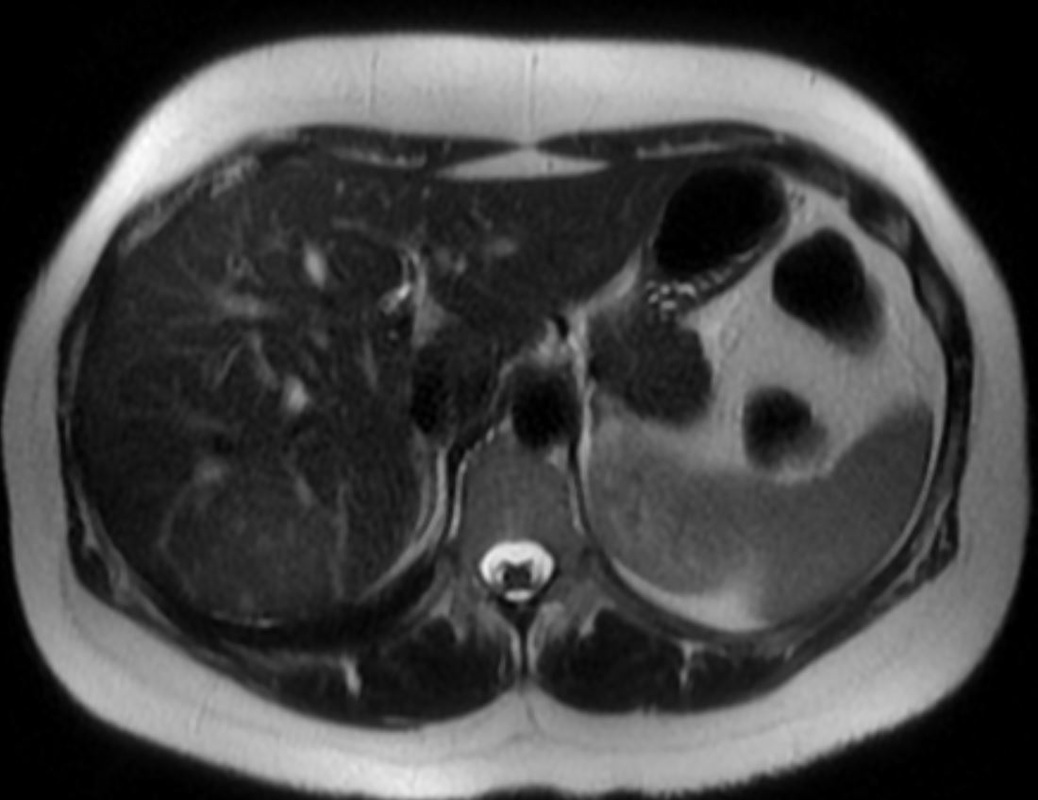
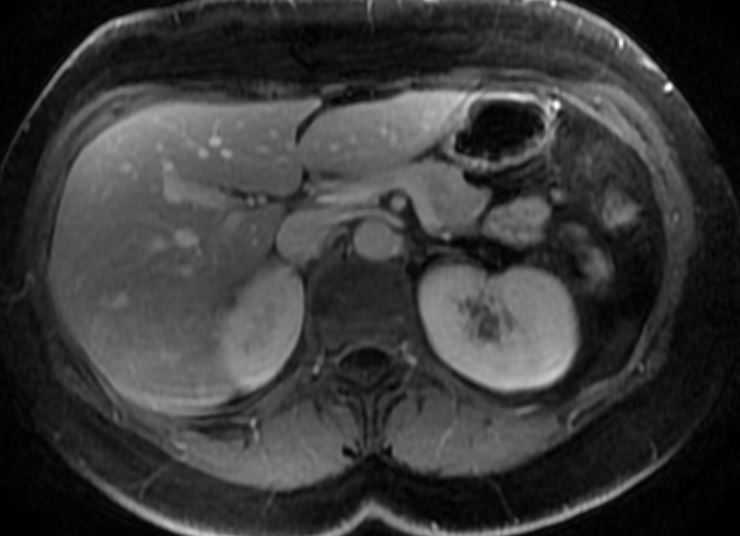
The sequences provided are in turn: T2 (short TE60ms), heavier T2-weighted (long TE120), T1, T1 fat suppressed gradient-echo arterial phase following conventional gadolinium contrast agent, portal venous phase, equilibrium phase.
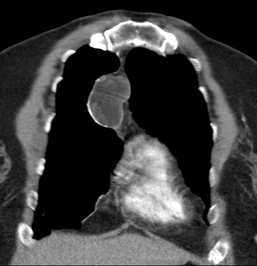
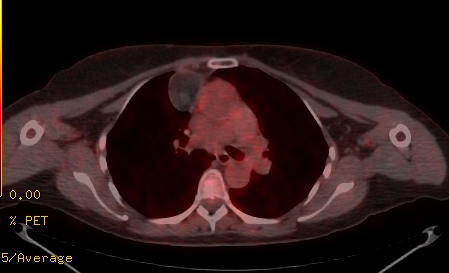
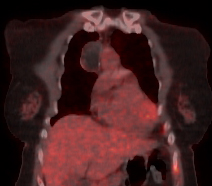
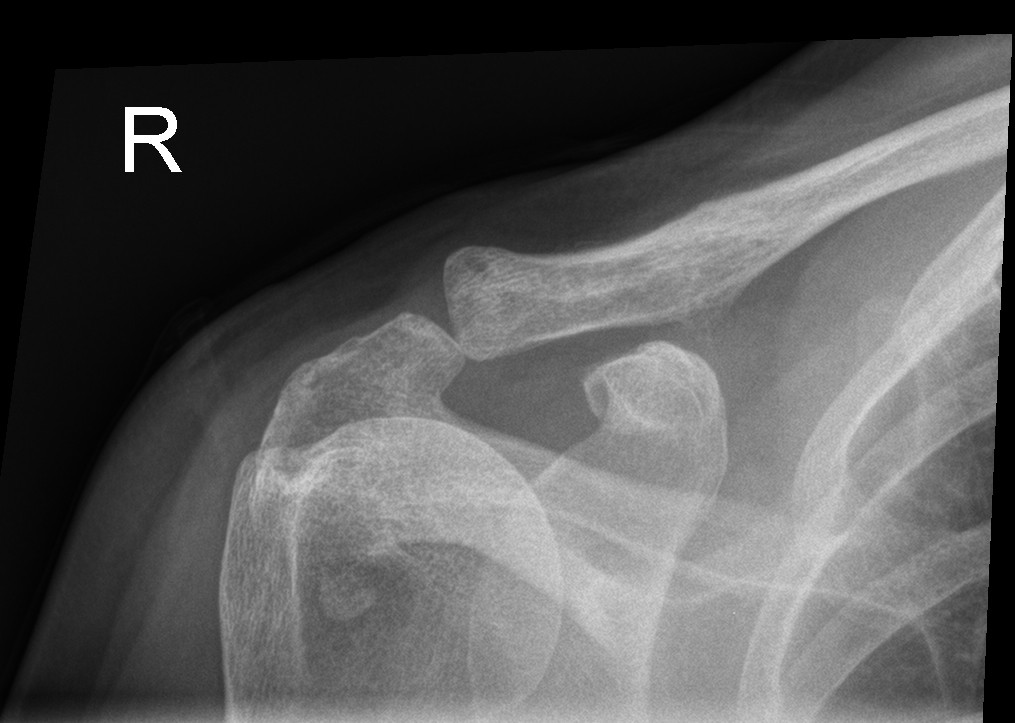
The initial T2-weighted images demonstrate a typically minimally T2 hyperintense abnormality demonstrating a slightly higher T2 central focus. Correspondingly this abnormality is largely isointense on T1 with a T1 hypointense central focus. Following contrast administration the lesion demonstrates diffuse heterogeneous enhancement with appearances that sometimes I think are somewhat comparable to a cut fruit, cauliflower or brain! This condition sometimes demonstrates a large artery extending to the central core, however, this is not present on the current examination. The equilibrium phase imaging demonstrates persistent mild hyperintensity that extends into the equilibrium phase. Notably the central region demonstrates progressive enhancement. These appearances are entirely specific for focal nodular hyperplasia, the diagnosis in this case. Although occasionally it is stated that fibrolamellar carcinoma can appear similar with a central scar, in practise fibrolamellar carcinoma is exotically rare and more typically presents with heterogeneous lesion, with areas of more prominent cystic liquefactive change and/or calcification. The enhancement of central scars in focal nodular hyperplasia typically in my experience is progressive from the outer rim of the scar to the central portion which may sometimes not completely enhance. The lesion typically demonstrates diffuse complete arterial enhancement of the non scar portion of the lesion with persistent mild enhancement in more delayed phases. This is the so called "mother in law phenomenon" (comes early,stays late). Minimal T2 hyperintensity of a subcapsular lesion is typical as this lesion is a hamartoma of normal hepatic parenchyma. The lesion if necessary can be confirmed by demonstrating uptake on 25-minute liver specific contrast agent MRI studies (gadoxetic acid). This is more typically required for lesions without an overt scar to differentiate then from adenomas or hypervascular malignant neoplasms (e.g. neuroendocrine). A relatively easy case. The chest radiograph demonstrates appearances of pneumomediastinum and surgical emphysema extending into the neck. The lung parenchyma is hyperinflated. At first inspection the lung parenchyma also demonstrates reticular markings, however, more careful inspection suggest these are actually diffuse cystic findings. The extent of cystic abnormalities discounts the possibility that these reflect bronchiectatic airways. It is notable that there is relative sparing of the lung bases. These findings are highly suggestive of the diagnosis.
The HRCT imaging at a later date is confirmatory. This demonstrates the extensive cystic distribution disease in the upper lobes, with relative sparing of the lung bases. Notably many of the cysts have a "bizarre" shape. Overall these appearances are highly suggestive of Langerhan's Cell Histiocytosis (Histiocytosis X). The appearances in this case are so suggestive on CXR that the HRCT is nearly superfluous! This disease appears almost exclusively in male smokers. Early forms of the disease may be associated with ill-defined nodules, these may progress to cavitary small nodules and eventually pure cystic disease. Early forms of disease can significantly improve or completely regress following cessation of smoking. Later forms of the disease can be more confusing as the cystic element may be less apparent and the confluent disease starts to resemble extensive reticular upper lobe fibrosis even on HRCT. The differential diagnosis for cystic lung disease is relatively limited. This can be considered in association with the size and distribution of cysts as well as the presence of nodules or ground glass: Differential: Cysts alone: Polycystic: 1. Langerhans 2. Lymphangioleiomyomatosis - no zonal predeliction, smaller uniform cysts, may see pneumothorax or rarely chylothorax, accessory features of tuberous sclerosis if co-present Oligocystic: 1. Lymphocytic Interstitial Pnemonitis (usually larger cysts at lung bases) 2. Remote post infective pneumatoceles 3. Birt-Hogg-Dube (rare - in association with renal tumours) Cysts and Nodules: Polycystic: Langerhans (early) Oligocystic Lymphocytic Interstitial Pnemonitis (small peri-cystic nodules may be present, if larger and more prominent consider the coexistance of LIP and amyloid) Cysts and Ground Glass: PCP infection |
From Grayscale
Latest news about Grayscale Courses, Cases to Ponder and other info Categories
All
Archives
October 2018
|





 RSS Feed
RSS Feed
