|
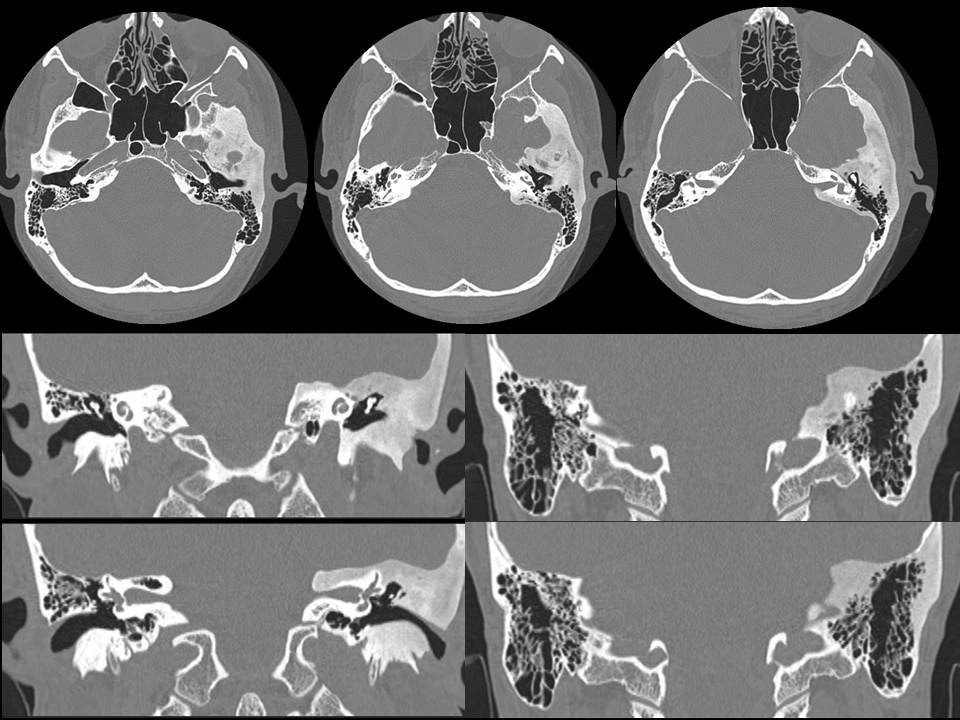
The images demonstrate asymmetric expansion of the left temporal bone which has a generalised ground-glass appearance. The cortex is intact. The trabeculae are not coarsened. The external auditory canal is narrowed on the left but is patent. Normal appearances of ossicular chains bilaterally. The middle ear spaces are clear. There is a symmetrical and normal appearance of the vestibulocochlear complexes. The appearances are diagnostic of fibrous dysplasia of the left temporal bone.
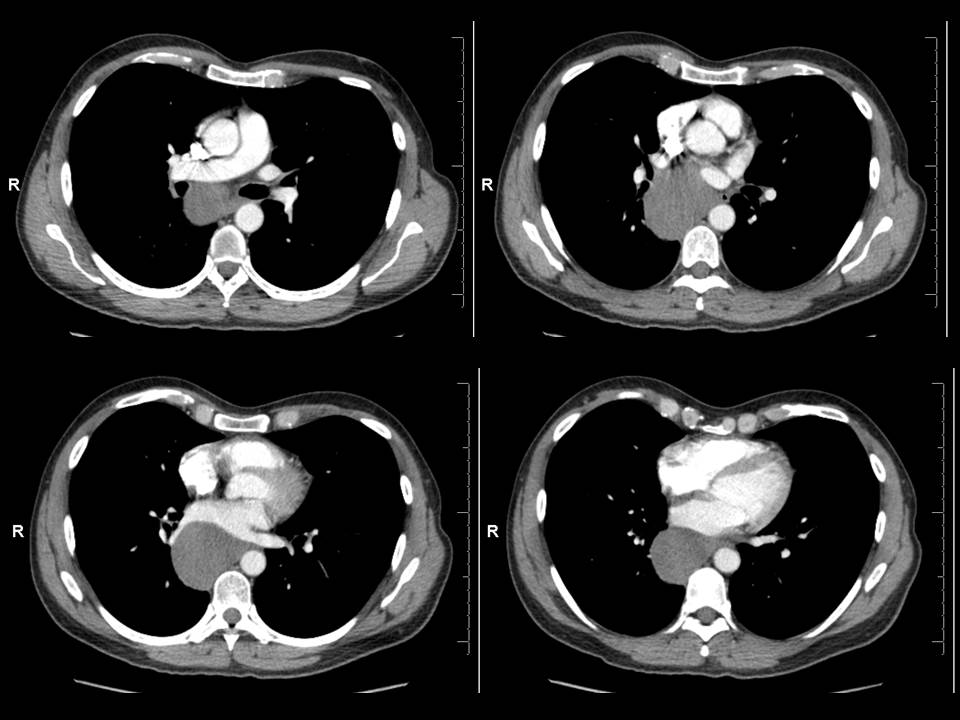
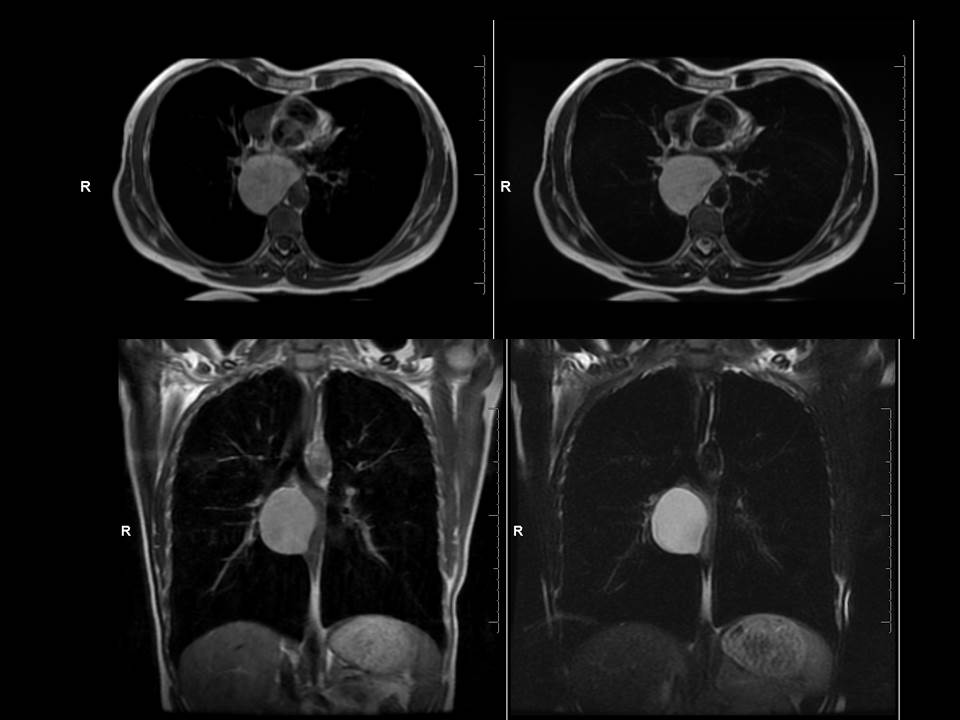
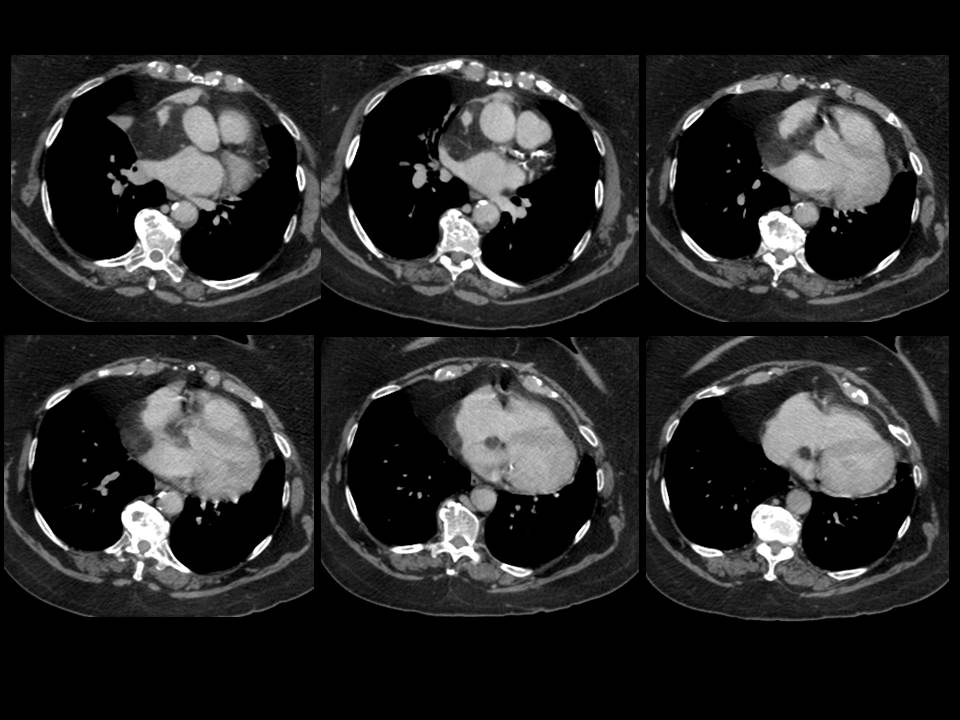
Craniofacial involvement in fibrous dysplasia may be considered a “monostotic” location despite involvement of several craniofacial bones or more rarely be part of a polyostotic fibrous dysplasia. Although more cases are monostotic, a higher proportion of polyostotic cases have craniofacial involvement (50%) versus craniofacial involvement in monostotic cases (25%) – although recall monostotic disease is overall more common. Within craniofacial fibrous dysplasia involvement of the anterior bones is more common than lateral or posterior bones with a recent study in the more sensitive CT era suggesting that ethmoidal involvement is the most common. Presentation may be asymptomatic/incidental, due to evolution of a lump or due to pressure effects. With regards to the temporal bone involvement of the external auditory canal as in this case may result in canal narrowing and conductive hearing loss. Involvement of the middle and ossicles does not usually occur although occasional cases of destruction of these structures have been described. This is usually the result of obstructive cholesteatomas that have been described following external canal occlusion. Inner ear involvement is also rare as is involvement of the facial nerve. Extension to the temporomandibular joint can cause joint deformity and present with trismus. Fibrous dysplasia has been described on plain films as pagetoid (ground glass opacity with small lucencies), sclerotic or cystic. However, these distinctions are not as clear at CT. Margins of involvement are variably described as well-defined or ill-defined, suggesting both can occur. In contradistinction to one of the main differential diagnoses, Paget’s disease, trabecular thickening or disruption of the cortex do not occur. Secondary aneurysmal bone cyst formation is a recognised complication. Diagnosis is based on typical appearances, predominantly at CT which also assists in differentiating fibrous dysplasia from other osteodystrophies of the skull base, including otosclerosis, osteogenesis imperfecta, Paget’s disease, and osteopetrosis. MRI may be of assistance (usually T1 intermediate, T2 helpful if low signal - a common manifestation- but can be heterogeneous including high signal too, heterogeneous contrast enhancement post Gadolinium). Treatment of this benign condition is usually conservative with partial surgical resection considered to relive pressure effects. Radiation is a historical treatment that is ineffective and was associated with sarcomatous degeneration. Case to Ponder 24: Lipomatous hypertrophy of the interatrial septum ("interatrial lipoma")21/7/2015 The abnormality is that of proliferation of fat in the interatrial space. This fat proliferation is epicardial within the pericardial space and does not arise from the septum itself. This causes separation of the walls of the left and right atrium except where they are inseparable, namely the fossa ovalis. This is a characteristic appearance. The lesion is not a genuine lipoma or neoplasm, simply fat proliferation that can confuse the unwary. The preservation of the fossa ovalis often results in a dumbbell like shape with an additional component medial to the fossa. This entity is an incidental finding sometimes found in obese patients or patients on steroid therapy or with mediastinal lipomatosis, although commonly none of these are present. It is best considered a benign incidental finding of no consequence. Although occasional cases have been described as causing mild dysrrythmias these links may be coincidental. Rare occurrences of superior vena cava compression have been described, I would imagine these were huge as for the most part these can be very large and yet asymptomatic. The most common association is that there may be proliferation of fat in the remainder of the epicardial space too - again inconsequential. On one occasion I have seen pericardial neoplastic infiltration spread through the space of the fat. This is an entity to recognise but to offer reassurance in dismissing it.
The humble plain abdominal radiograph of the abdomen is all that is needed here. The ascending colon and transverse colon are dilated by air but also by mottled density suggestive of liquid stool. The mucosa though of this segment of the large bowel is unremarkable and there is no bowel wall pneumatosis or free air. There is an abrupt transition at the splenic flexure to completely decompressed descending colon. This segment of the large bowel has no haustra and can be seen to be markedly thickened throughout its length, standing somewhat proud of the properitoneal fat plane lateral to it, likely due to further pericolonic inflammation. These are typical features of a colitis. The distribution would be atypical for an ischaemic colitis and more favourable for inflammatory bowel disease (Ulcerative Colitis or less likely Crohn’s) but also one should consider infectious colitis such as pseudomembranous colitis.
First case for Sept course registrants went out by email today. Personalized responses for your thoughts. Please email me if you have not received your case at [email protected]
Select places still available for Sept 5-6 and Sept 12-13 courses. The appearances are of a single well defined unilocular lucent lesion with a fine cortical rim in the mandibular ramus. The patient is adult and there are no unerupted teeth in the vicinity of the lesion. By definition this is, therefore, considered a non-aggressive lesion. Despite this there is medial deficiency of the mandibular cortex. In this medial location a well defined lesion appearing to invaginate into the osseous cortex is reminiscent of a Stafne’s cyst. Stafne’s cysts are intraosseous herniated inclusions of the submandibular or sublingual glands into the mandible. In this case there is no connection to the submandibular gland and the attenuation of the cystic component is less than that of the submandibular gland. However, Stafne’s cysts can arise from accessory glands and their attenuation can vary from that of the remainder of the salivary glands. Indeed this would be a typical location occurring between the first molar and the angle of the mandible. Typically Stafne’s cysts are asymptomatic discoveries rather than presenting with pain as in this case. However, more critically Stafne’s cysts occur below the inferior alveolar nerve canal. Reviewing the orthopantomogram and the curved planar reformat it is evident that this lesion lies above the inferior alveolar nerve canal. In addition one can identify that there is a connection to the empty nerve root of a removed molar. This suggests that the findings are far more likely to be due to a radicular cyst, synonymous with a periapical cyst. These lesions arise initially as an apical (near the apex of the roots) periodontitis related to chronic careous change or dental root treatment. A subsequent granulomatous response results in a small (<1cm) round or ovoid cyst with a thin walled cyst that like most dental related lesions arise above the inferior alveolar nerve canal in the mandible.
|
From Grayscale
Latest news about Grayscale Courses, Cases to Ponder and other info Categories
All
Archives
October 2018
|

|
|
Grayscale Courses est. 2015


 RSS Feed
RSS Feed
