|
Spaces still available on Sep 5-6th and Sep 12-13th Courses.
0 Comments
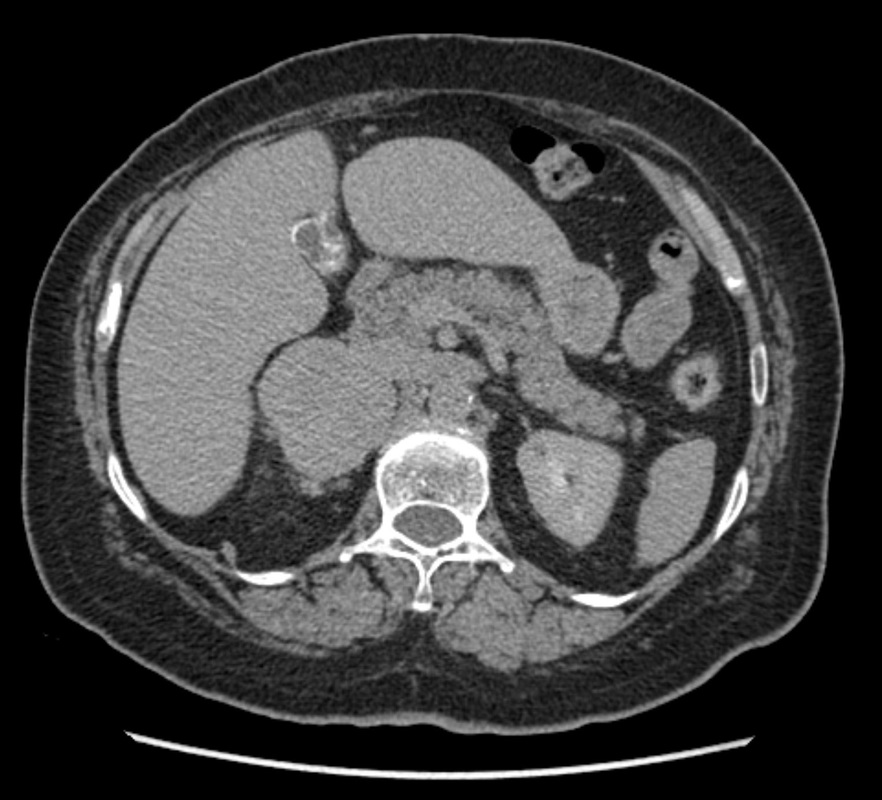
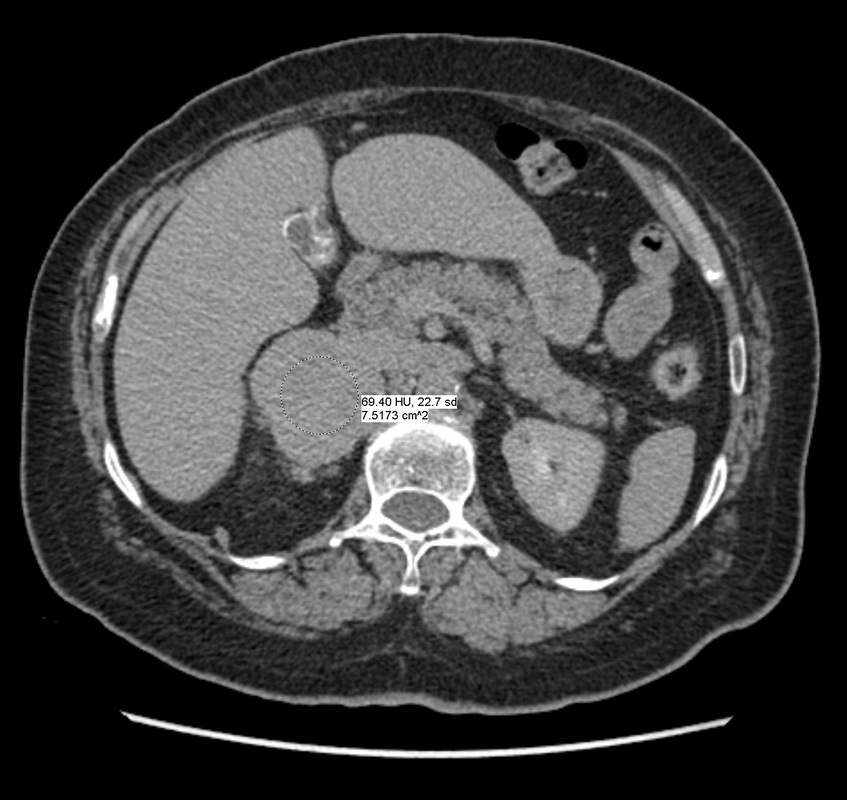
What not an adenoma!?
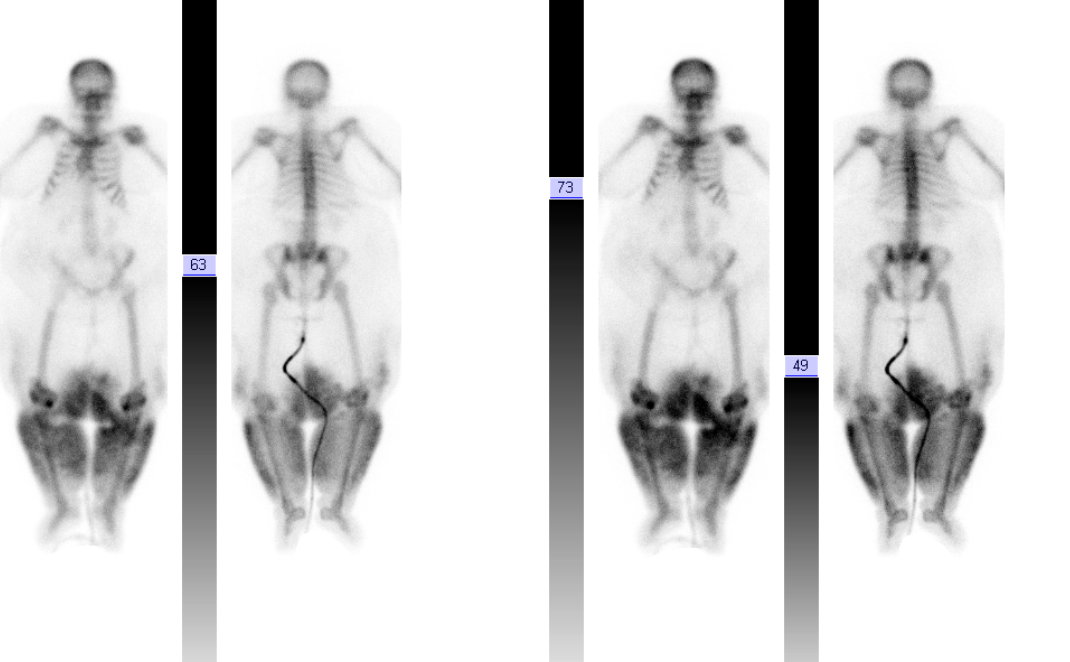
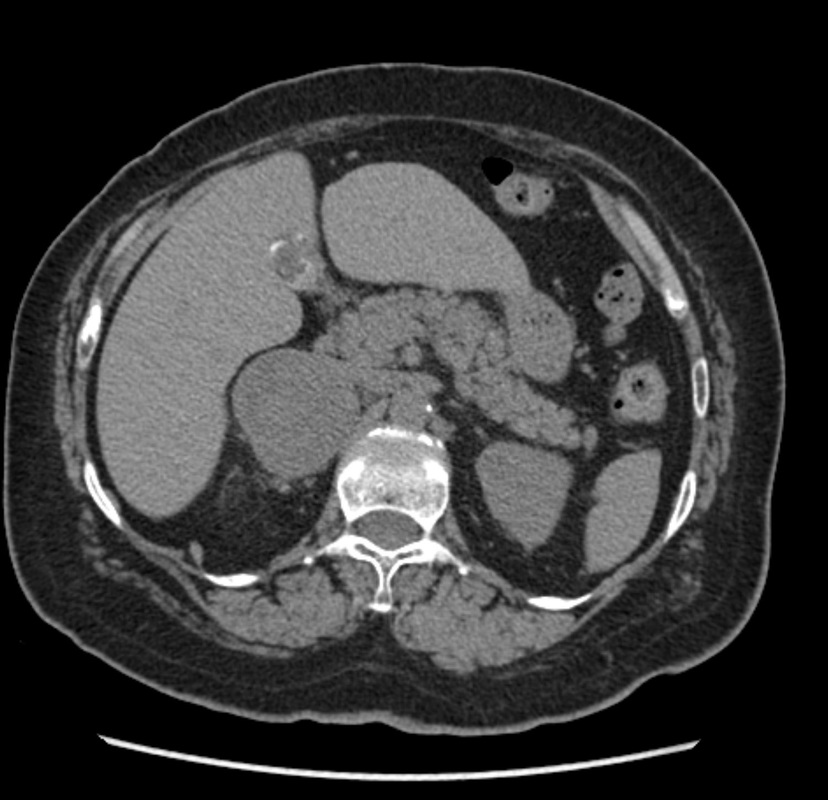
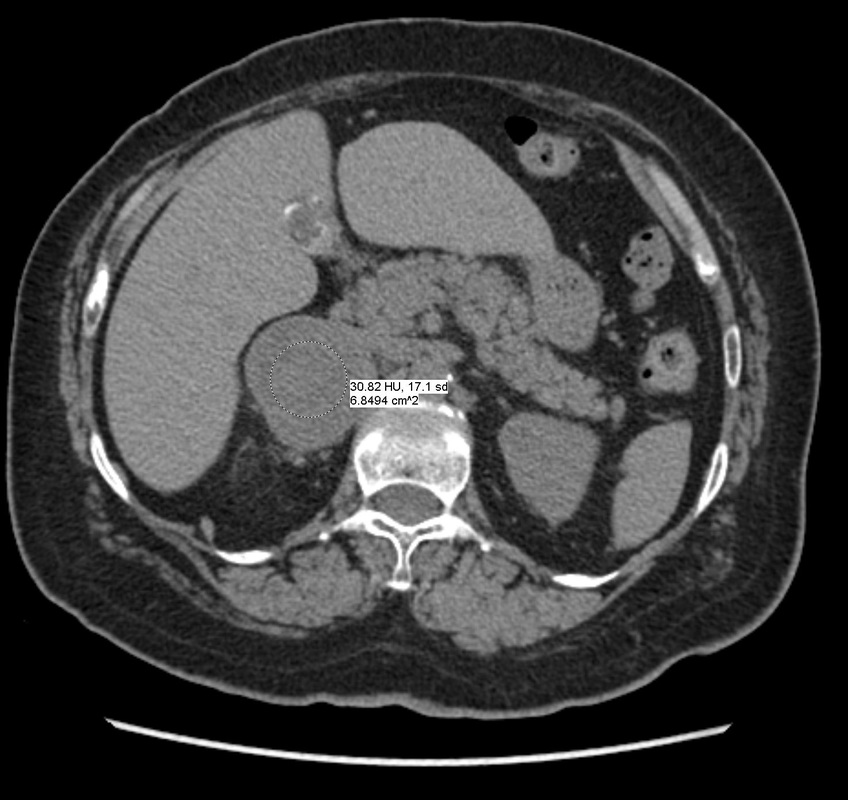
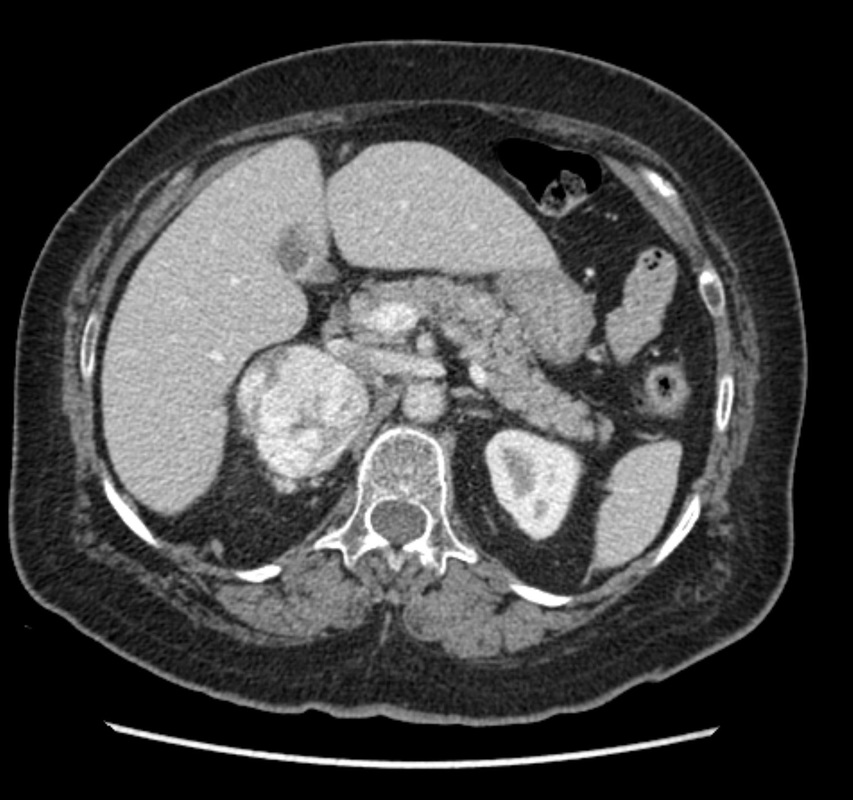
The imaging provided demonstrates a CT adrenal washout study. CT adrenal washout studies are performed for lesions that do not satisfy diagnostic criteria for demonstrating the presence of lipid rich adenoma either by non contrast CT or by MRI paired T1 in and out of phase imaging. Note that it is a common error to perform an MRI examination following a non contrast CT examination that demonstrates CT Hounsfield units greater >10 HU, or inversely to perform a non contrast CT following the MRI examination that does not demonstrate significant signal dropout. As these tests are both evaluating the same physical characteristic, namely the presence of intra voxel fat, a surrogate of microscopic fat, there is no additional diagnostic benefit in performing both examinations. CT adrenal washout studies are performed by performing a non contrast examination to establish the baseline attenuation of the adrenal lesion. A subsequent portal venous phase acquisition is performed, supplemented by a 15-minute phase evaluation. In principle benign adrenal adenomas, including those that are lipid poor, measuring >10 HU at baseline, will demonstrates significant enhancement and subsequent de-enhancement (washout). Malignant tumours demonstrate enhancement but less washout. It is important that measurements are performed with a representative region of interest (ROI) that encompasses generally greater than 70% of the lesion on the sections best demonstrating the lesion, rather than utilising small ROIs that may selectively demonstrate one region. Within larger lesions, however, it is prudent to perform more than one confirmatory large ROI measurement. Absolute washout is defined as the following (PV=Portal venous, Pre=Precontrast): 100 x (PV HU - Delayed HU)/ (PV HU - Pre HU). >60% suggests adenoma (sens 86%, spec 92%). It is possible to also to consider only the portal venous and delayed phase (e.g. this is sometimes helpful with incidnetal adrenal nodules in two phase CT colonography studies). This results in relative washout measurement which is defined as: Relative washout: 100 x (PV HU - Delayed HU)/ PV HU. >40% suggest adenoma (sens 82%, spec 92%). Therefore, in this instance the lesion demonstrates an absolute washout of 67% and relative washout of 53%, both of these suggesting a benign adenoma. However, there are certain caveats to CT adrenal washout studies. Firstly the studies that evaluate both densitometry washout of adrenal nodules generally evaluated smaller lesions, measuring 3 cm or less. The probability of neoplasia in larger adrenal lesions is significantly higher, particularly as lesions exceed 5-6 cm. Heterogeneous lesions are also more likely to be neoplastic. Finally it is also important to consider that an adrenal lesion that measures more than 120HU on the portal venous phase acquisition is highly likely to reflect a malignant metastasis (particularly hepatocellular carcinoma or renal cell carcinoma) or phaeochromocytoma. There is also well recognised a minority phaeochromocytomas may also mimic the washout characteristics of lipid poor adenomas. In this case the marked heterogeneous enhancement and large size of the tumour with PET portal venous enhancement greater than 120 HU highly suggested phaeochromocytoma which was the ultimate diagnosis confirmed from urinary metanephrines. The initial shoulder x-ray demonstrates no significant abnormality of the shoulder. In general it is better to consider a shoulder radiograph as a small chest radiograph! The pathology you may observe in the chest is highly likely to be more significant than that in the shoulder joint. This is a common site for radiographic misinterpretation, with pulmonary parenchymal nodules including neoplasm frequently missed while minor degenerative changes of the acromioclavicular joints are expounded upon. So for every shoulder chest radiograph please review any portion of the chest first.
Bearing in mind this advice it is clear that the extended shoulder chest radiograph demonstrates an abnormal contour of the right side of the mediastinum. Loss of the ascending border of the aorta is present consistent with an anterior mediastinal mass abnormality. This is a further depicted on the subsequent chest radiograph which demonstrates the appearances of the "hilum overlay" sign with normal visualisation of the right hilar vessels. These are visualised distinct from the mediastinal mass which is anterior in the mediastinum. The subsequent CT examination demonstrates this mass lies along the right antero-lateral margin of the anterior ascending aorta and contains extensive areas of mature fat with peripheral linear minor calcification and some smaller nodular elements. The accompanying PET examination demonstrates that there is no FDG activity within this region. In order to define the aetiology of this abnormality ibe has to also consider the patient age. This patient is an elderly and therefore aggressive fat containing anterior mediastinal tumours (principally immature teratoma is and rarely liposarcomas) are unlikely.Immature teratoma are far more likely in young male patients. Diagnostic considerations might include a thymolipoma or more likely based on heterogeneity and calcifications a mature dermoid. In this particular instance the lesion was resected and the diagnosis proved to be a mature cystic teratoma of the thorax. Mature cystic teratoma of thyroid can be considered to be a variant of mature dermoid of the pelvis. There is a rare association of mature teratoma with Klinefelter's syndrome, however, the vast majority of cases are not associated with this syndrome. These lesions have absent/very low malignant potential and often contain exclusively ectodermal and mesodermal cells (squamous epithelium/skin) rather than the three embryological layers present in most immature teratoma tumours (endoderm, mesoderm, ectoderm). Immature teratomas have malignant transformation risk. All teratoma lesions usually arise in or near the body of the thymus and are usually well demarcated lesions that may displace rather than invade other mediastinal structures. As in this case they are frequently asymptomatic and incidentally detected. They may contain fat or calcifications - heterogeneity is common. Complete excision is required to definitively exclude malignant potential. In general cystic lesions tend to be benign whereas lesions with solid material are more likely to be immature teratomas or undergo malignant transformation. Even mature teratomas have a small risk of malignant transformation to a malignant germ cell tumours. Additionally even more rarely secondary somatic cell malignant transformation can occur in the non germ cell components of mediastinal mature teratomas resulting in carcinoma, sarcoma or leukaemia. |
From Grayscale
Latest news about Grayscale Courses, Cases to Ponder and other info Categories
All
Archives
October 2018
|

|
|
Grayscale Courses est. 2015

 RSS Feed
RSS Feed
