|
Level: ABR, EDiR, FRCR, Radiology Mid-Level ++
1 Comment
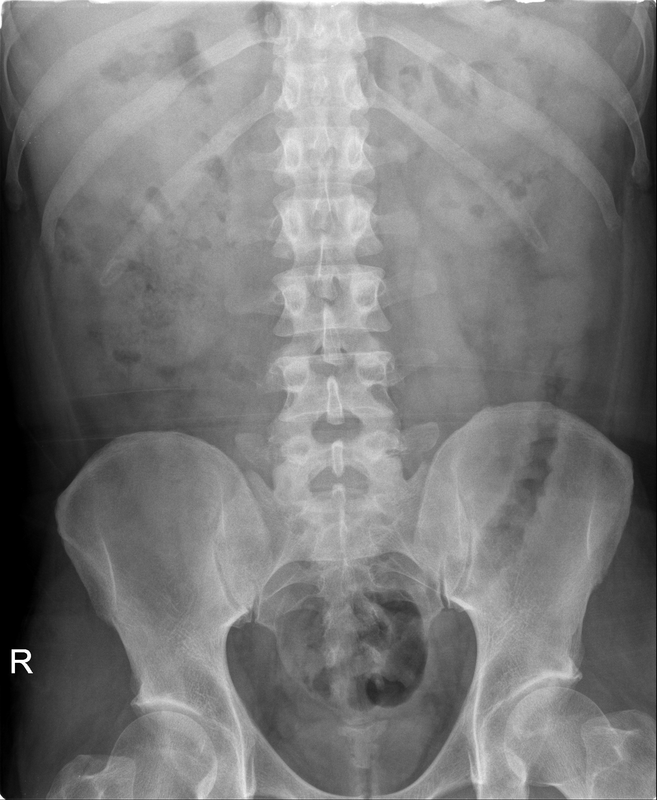
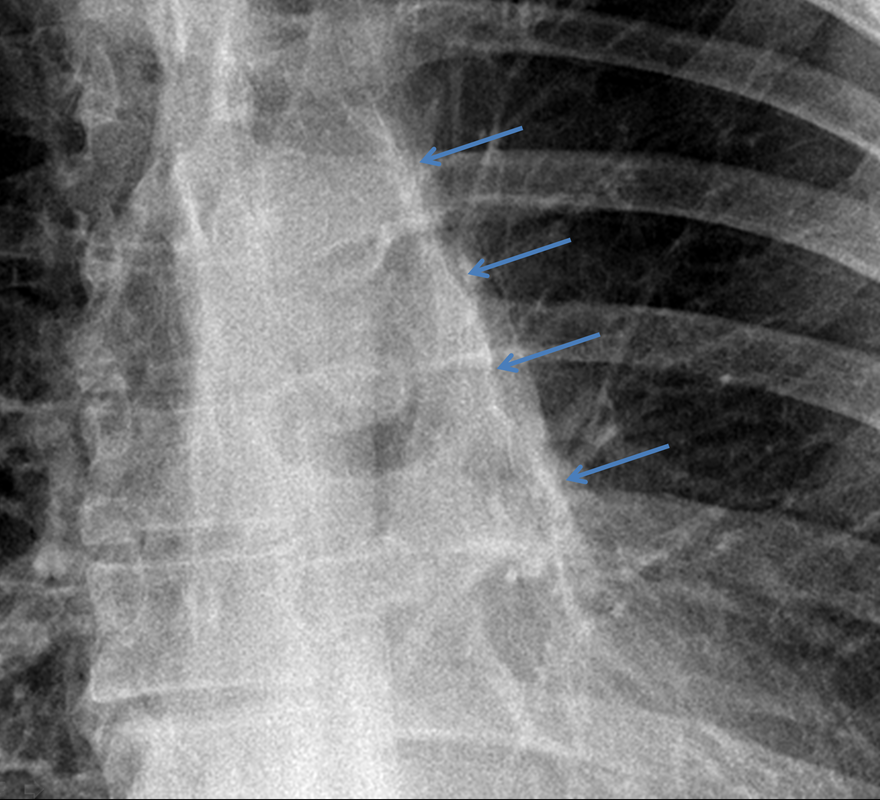
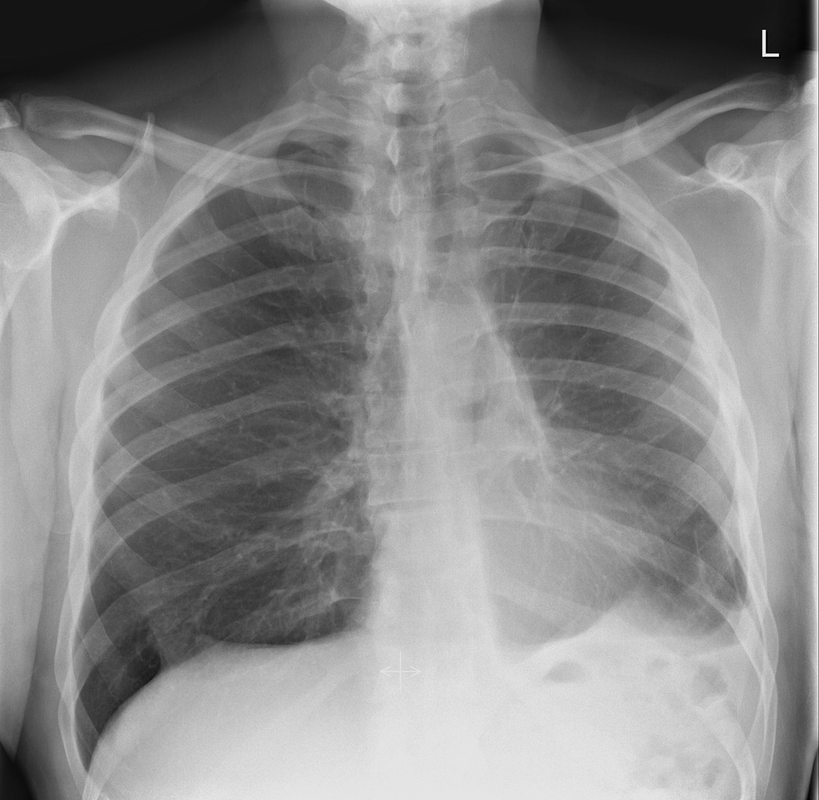
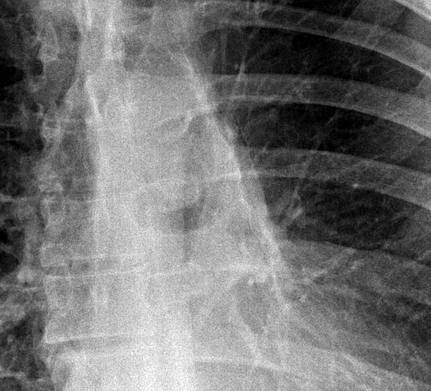
Level: EDiR, ABR, FRCR Radiology Mid-Level ++ This case is a companion case to the Case 64, with many comparable features, many of which are more pronounced than the prior case. The left hemithorax is contracted with shift of both the superior and inferior mediastinum to the left. Comparable to the prior case there is also evidence of selective volume loss in the left upper thorax with elevation of the left hilar structures, a horizontal orientation of the left main bronchus and tenting of the left hemidiaphragm. However, in contradistinction to the prior case there is no perihilar opacity present. So this appears to reflect extreme left upper collapse but with no residual opacity visible to reflect the collapsed left upper lobe. There is an additional feature present. This is a fine line of high attenuation material running parallel to the mediastinal surface in the left perihilar region (arrow). The appearances are those of chain sutures as part of a left upper lobectomy which accounts for the volume loss differences demonstrated.
Lobectomy can be a difficult diagnosis to make. Appearances often mimic the characteristic appearances of lobar collapse but are lacking in the typical opacities that result from the collapsed lung parenchyma. Surgical clips are often conspicuous by their absence as these are rarely used or of a large enough size to be visualised on plain radiographs. Chain sutures can be variably used as in this case and be identified. These are used to complete an incomplete fissure and create a dividable plane so as to enable an air-leak free plane for an anatomical resection of the lobe. They can be difficult to see as they are so fine, resebling a very fine interlinked chain necklace. They are best visualised by magnification and sometime sharpening the image display. Post-operative changes of the ribs may also be appreciable, although this was more common in remote cases where a more extensive periosteal stripping was utilised that resulted in an irregular rib re- growth. In modern thoracotomy the rib irregularity is very focal and can be so subtle as to not even be identifiable even at CT. In post-lobectomy patients a small pleural effusion and persistent pleural thickening is often present at the lung bases, resulting in a long-standing pleural reaction. Determining the lobe of resection on plain radiographs relies on determining the position of the hilum and the central bronchovascular structures with expected superior displacement for upper lobe resections and conversely inferior displacement for lower lobe resections. Level: MRCP, ABR, EDiR, FRCR, Radiology Junior +
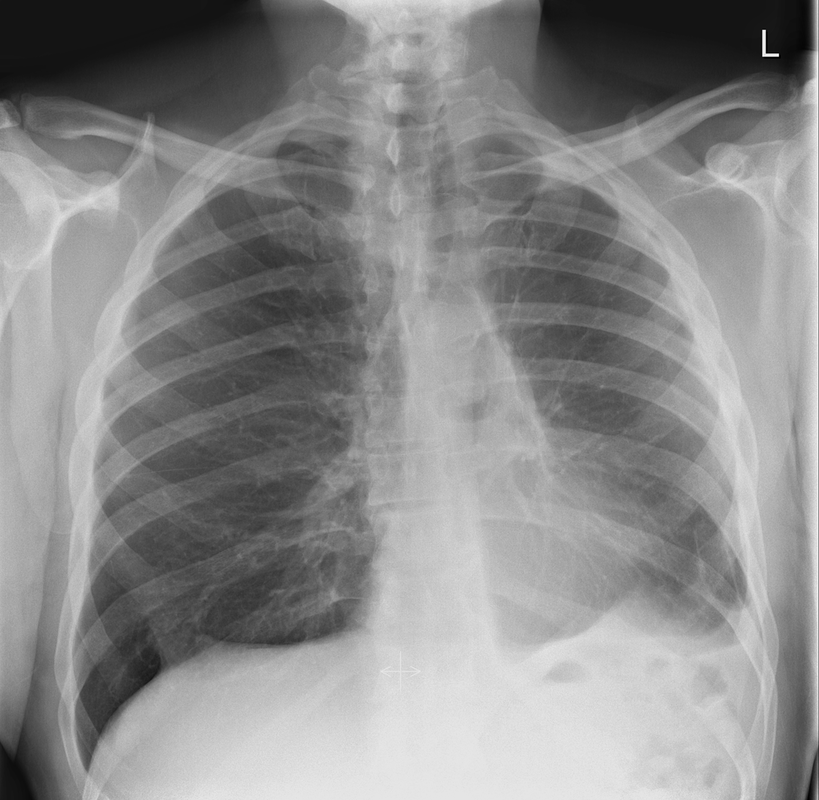
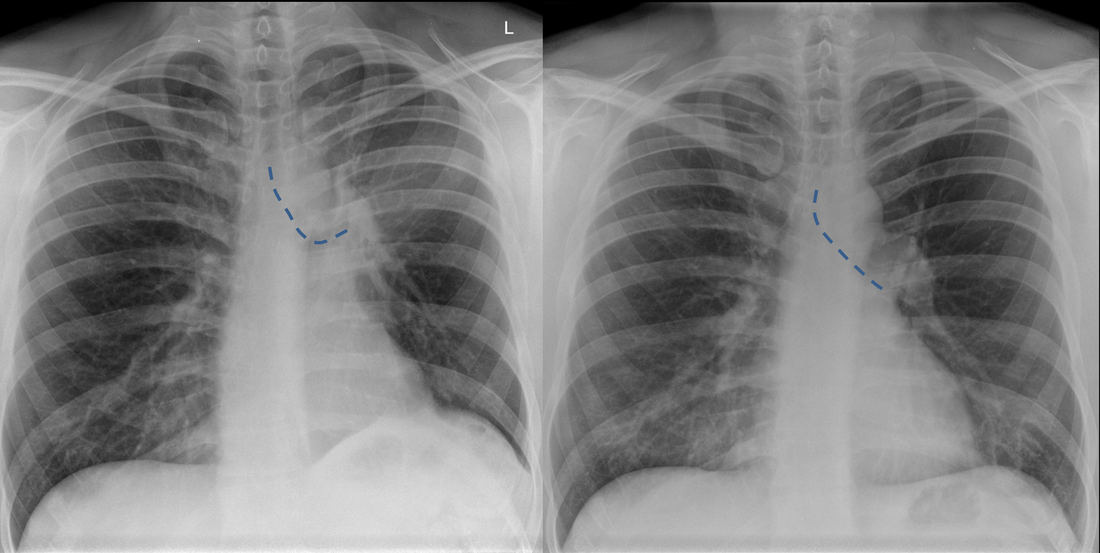
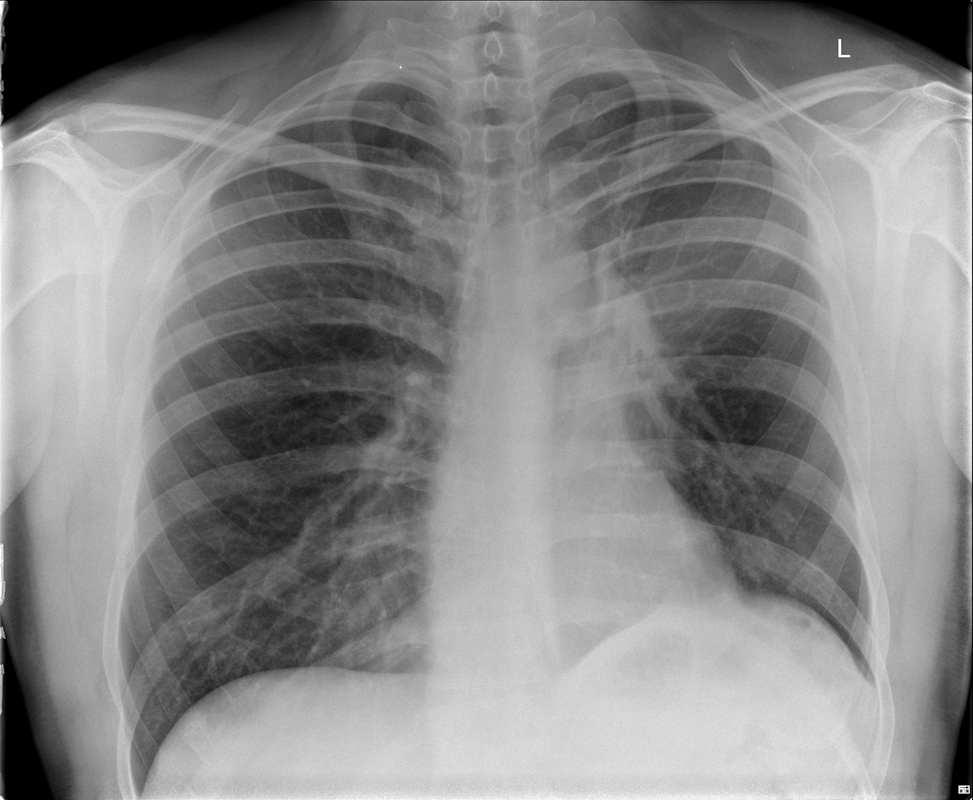
The current chest radiograph is clearly abnormal, the prior chest radiograph provided for comparison was normal. The current chest radiograph demonstrates left perihilar opacity denser centrally, fading towards the periphery. There is a retained lucency medially, lateral to the aortic arch. The left hilum is elevated. Note also that the left main bronchus (dotted line) is now horizontal, compared to the oblique normal orientation on the prior film. The left hemidiaphragm is slightly more elevated and the cardiac silhouette slightly more displaced to the left, not now protruding to the right of the spine. These characteristic appearances are all indicative of volume loss in the upper left hemithorax, specifically left upper lobe collapse.
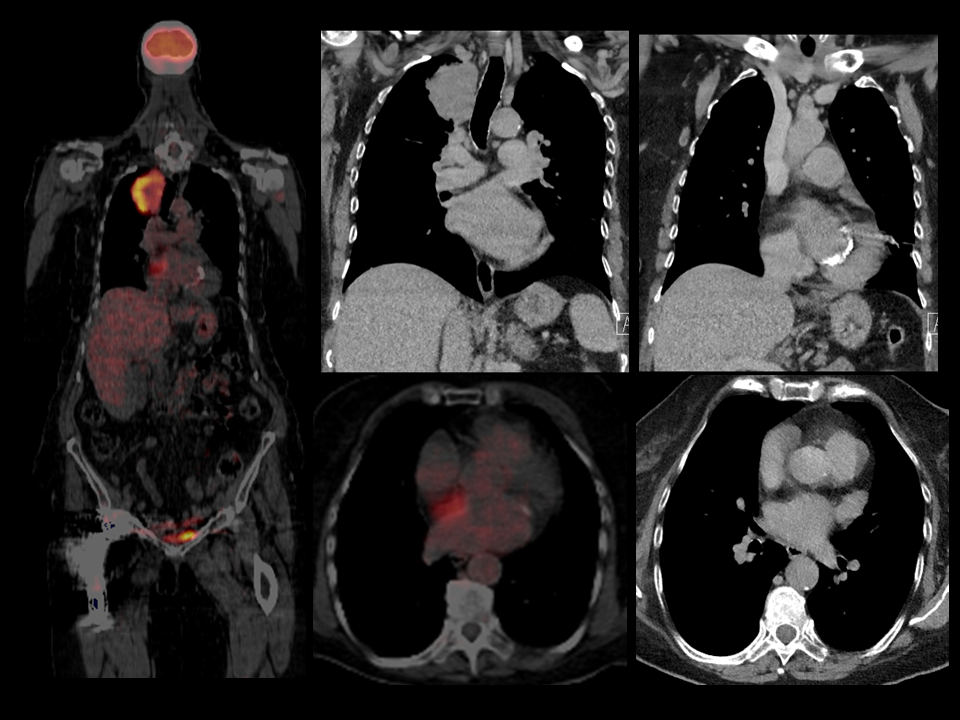
In left upper lobe collapse, the left upper lobe collapses anteriorly. This anterior movement of the collapsed lung is greater peripherally and more restrained by the hilar attachment medially. So centrally density is retained and peripherally this fades. When the lung is minimally collapsed the entire left lung may demonstrate diffuse opacity through which vessels are still seen in the lower lobe. These appearances are the so called “veil like” opacity. As the collapse progresses, as in this case, the opacity contracts towards the hilum. Paradoxically, the opacity generated by the collapse reduces as the severity of the collapse increases. In these instances it is important to assess ancillary features of volume loss to differentiate the perihilar opacity of collapse from a mass. In this case the loss of volume in the left hemithorax is supported by the cardiomediastinal shift and the minor elevation of the left hemidiaphragm. In general terms upper lobe collapses tend to cause shift of the upper mediastinum whereas lower lobe collapses cause greater shift of the lower mediastinum and heart, although, as in this case, that is inconsistent. Tenting of the diaphragm, sometimes termed a juxtaphrenic peak, can also occur due to attachments of the hilum to the inferior pleural surface via an inferior accessory fissure or less frequently an inferiorly extending inferior pulmonary ligament. Generally, unless dealing with extreme long-standing fibrotic upper lobe collapse, significant elevation of the hemidiaphragm is unusual. If there is significant elevation it is important to consider that the collapse is due to a malignancy with infiltration of the phrenic nerve. The upper lobe collapse is confirmed by elevation of the hilum and loss of clarity of the previously visible left pulmonary artery. The horizontal nature of the bronchus, further adds weight to the upper volume loss. Finally, a specific feature supports the left upper lobe collapse. That is the peri-aortic lucency, often termed the “Lűftsichel sign” (sickle of air). This is appearance is due to superior herniation of compensatorily hyperinflated left lower lobe lung parenchyma medial to the collapsed left upper lobe. In this case the collapse was due to an entirely endobronchial carcinoid tumour with none of the opacity visualised in the perihilar region due to tumour but all due to left upper lobe collapse. Case to Ponder 63 Answer: T4N0 Lung Carcinoma with Hypermetabolic Interatrial Lipomatous Hypertrophy12/5/2016 Level: ABR, FRCS, MRCP, EDiR, FRCR, Radiology Senior +++ This case demonstrates axial and coronal fused PET-CT images as well as non-contrast corresponding CT images from a contemporaneous examination. The images demonstrate a large mass in the right upper lobe. This invades the mediastinum medially. This appearance is that of a T4 lung carcinoma.
Within the mediastinum there is an area of activity on the coronal PET-CT images. This does not correspond to a typical nodal station. Coronal and axial images demonstrate that this is within the region of the interatrial septum. There is a proliferation of fat in the inter-atrial septum. This is benign inter-atrial lipomatous hypertrophy. The fat in this region can have hyper-metabolic brown fat properties much like fat in the root of the neck. Metastatic disease can spread through this region, however, only in contiguous locally advanced intra-pericardial tumours. This case should have been no challenge to those paying attention to earlier cases (see January 2016 cases , Case to Ponder Number 52 for more information: http://www.grayscalecourses.com/news-cases/archives/01-2016 Level: EDiR, FRCR, MRCP, Radiology Junior + The chest x-ray demonstrates multiple abnormalities. Overall the lung volumes are increased with flattened diaphragms, likely due to chronic air-trapping from COPD. However, in addition bilateral upper lobe volume loss is present due to scarring. Note the bilateral apical pleural thickening, the elevation of both hilar regions and the tenting of both diaphragms. The volume loss is greater in the right upper lobe with greater elevation of the right hilum and tracheal deviation to the right. There are multiple patchy parenchymal opacities which are most pronounced in the upper and mid-zones, reflecting the fibrotic inflammatory process. These appearances are most suggestive of a fibrotic inflammatory process such as chronic tuberculosis.
The left upper lobe also demonstrates a large thick walled tuberculous cavity. These are not uncommon but in this case the cavity is large and contains a heterogeneous attenuation mass with mottled air within it. Superior to the intracavitary mass there is a lucency of air. This appearance is typical of a mycetoma, due to Aspergillus, synonymously termed an Aspergilloma. Such Aspergillomas are typically due to Aspergillus fumigatus, a non-invasive form of pulmonary Aspergillosis. They occur in immune competent patients as a saprophytic secondary infection in areas of pulmonary destruction, chronic scarring or typically cavities. Tuberculous cavities, scarring from sarcoidosis or cystic bronchiectasis are the commonest substrates for the disease to form. The infection is often preceded by progressive pleural focal thickening. Subsequently a fungus ball of hyphae forms. This is free within the cavity and can be demonstrated to re-position on decubitus positioning at CXR or CT. Above the hyphal ball there is a lucency of air within the cavity. This is often referred to as “an air crescent”. Confusingly this term of "air crescent" is also sometimes used in patients with invasive aspergillosis. However, in contradistinction invasive aspergillosis occurs in neutropenic immune compromised patients. In that instance the air-crescent develops in during the neutropenic recovery phase in areas of focal air-space opacity that have developed in areas of previously normal lung. Frank cavities can form later, but they are the sequela of an invasive form of the disease not a secondary manifestation within chronic cavities. The crescent of air in Aspergilloma is also occasionally referred to as the Monod or Monad sign by purists but most will never have heard of this terminology! The mortality of Aspergilloma is variable but usually low even if medical therapy fails and surgery is required. The Aspergilloma contains hyphae, cellular debris and some granulation tissue. As a result of the chronic inflammation hypertrophy of the bronchial arteries can occur and result in haemoptysis, occasionally massive. This can be treated by selective angiographic embolization. For completeness, the lung can of course be affected by two more variations of aspergillus. The semi-invasive form of Aspergillus occurs in patients with minimally reduced immunity (e.g. chronic poor nutrition, alcoholics etc). It results in chronic air-space opacities that can be difficult to differentiate from other causes of chronic infection or organising pneumonia. The allergic phenomenon of allergic bronchopulmonary aspergillosis is an exaggerated hyper-immune response to Aspergillus typically in patients with asthma. It results in central bronchiectasis with mucoid impactions, sometimes referred to as “finger in glove” when branching from the hilum. |
From Grayscale
Latest news about Grayscale Courses, Cases to Ponder and other info Categories
All
Archives
October 2018
|

|
|
Grayscale Courses est. 2015




 RSS Feed
RSS Feed
