|
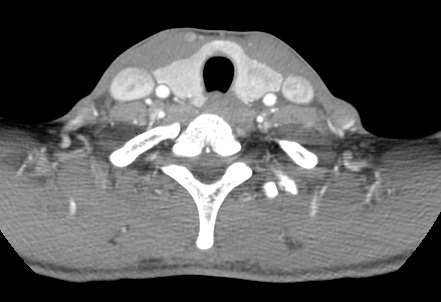
The 123I-MIBG examination demonstrates increased uptake in both adrenal glands, persistent at 24 hours. In addition, subtle uptake is noted in the region of the left thyroid gland. The CT examinations provided demonstrate that there are bilateral heterogeneously enhancing lesions in the adrenal glands, larger on the right side and smaller on the left side. These findings in conjunction with the MIBG examination are highly suggestive of bilateral adrenal phaeochromocytomas. In addition a left thyroid nodule is appreciated on the CT examination. This appearance is nonspecific, however, in conjunction with the 123I-MIBG examination demonstrating increased uptake in this region the diagnosis of the medullary cell carcinoma as part of MEN2a (multiple endocrine neoplasia) is the likeliest diagnosis.
In MEN2a phaeochromocytomas are present in half of patients, ofen bilateral or extra-adrenal. By definition 100% of patients also have medullary thyroid carcinoma, although this may present before after the phaeochromocytoma. In addition, approximately 20% of patients may demonstrate hypercalcaemia due to hyperparathyroidism. On CT imaging this may manifest as renal calculi or foci of medullary calcinosis. Most cases of MEN2 are due to variable mutations of the RET proto-oncogene which controls TGF-beta (transforming growth factor beta) which is critical to neural development. Although autosommal dominant in transmission, expression is variable and approximately 50% of cases are due to new mutations. MEN2a is closely related to MEN2b which demonstrates additional marfanoid body habitus and mucosal neuromas/ganglioneuromas often perioral. It is distinguished from MEN1 which is an autsomal dominant syndrome typically presenting with primary hyperparathyroidism but also demonstrating islet cell tumours in approximately half of patients and pituitary adenomoas in approximately 30% of patients. A common association to consider for MEN1 is when identifying an islet cell tumour (usually gastrinomas but also glucagonomas or insulinomas) that "incidental" renal calcifications or stones my be a reflection of MEN1 (PPP, Parathyroid/Pituitary/Pancreas). MIBG imaging can be used to localise phaeochromocytoma, to determine whether a mass is due to a phaeochromocytoma or to exclude metastatic disease. For adrenal phaeochromocytoma MIBG specificity is approximately 100% with lower sensitivity (86%). In practice therefore the combination of CT or MRI with MIBG is near 100% sensitive. Octreotide as alternative agent has inferior sensitivity (20-50%) compared to MIBG for adrenal phaeochromocytoma but has superior sensitivity for extra-adrenal phaeochromocytoma (96% versus 72%).Octreotide is therefore sometimes preferred for MIBG negative examinations or head and neck evaluations. Both agents may be used with reduced sensitivity to detect medullary thyroid carcinoma. 123MIBG is sometimes used to establish uptake prior to therapeutic 131 MIBG treatment. The courses of Sept 5-6th and Sept 12-13th were a great success! Great candidates on both weekends. It was very intensive and educational. We saw 200-300 cases! Above all we all worked together and it was a lot of fun. Best of luck to all
|
From Grayscale
Latest news about Grayscale Courses, Cases to Ponder and other info Categories
All
Archives
October 2018
|

|
|
Grayscale Courses est. 2015



 RSS Feed
RSS Feed
