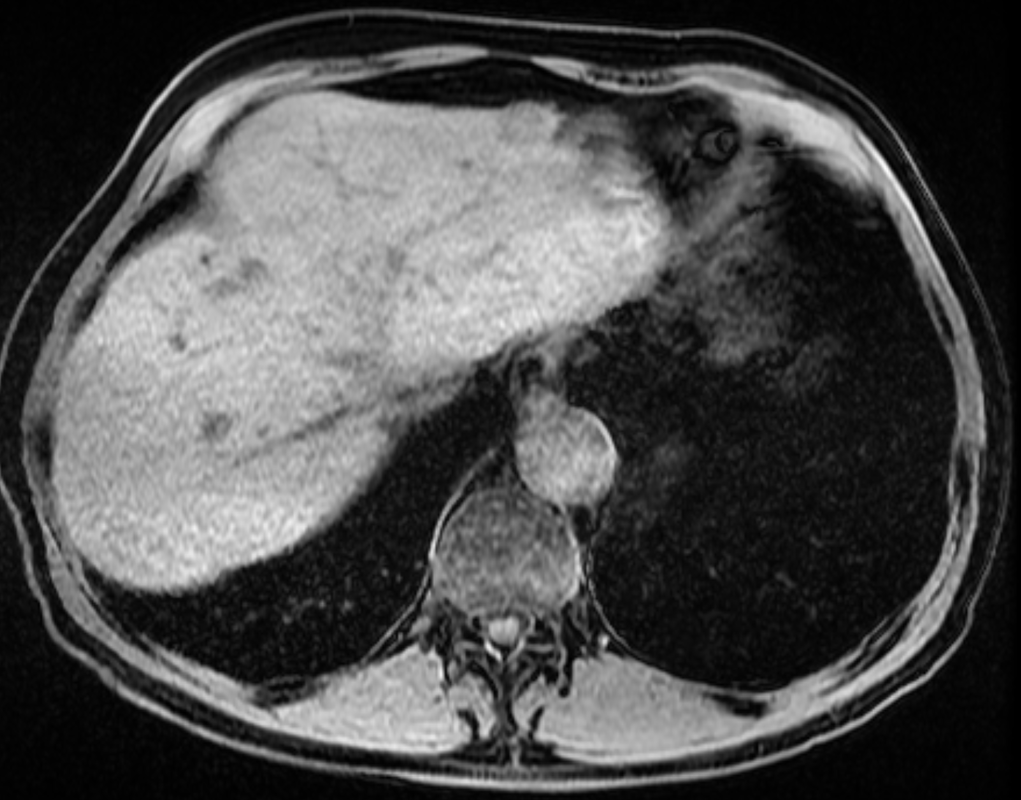
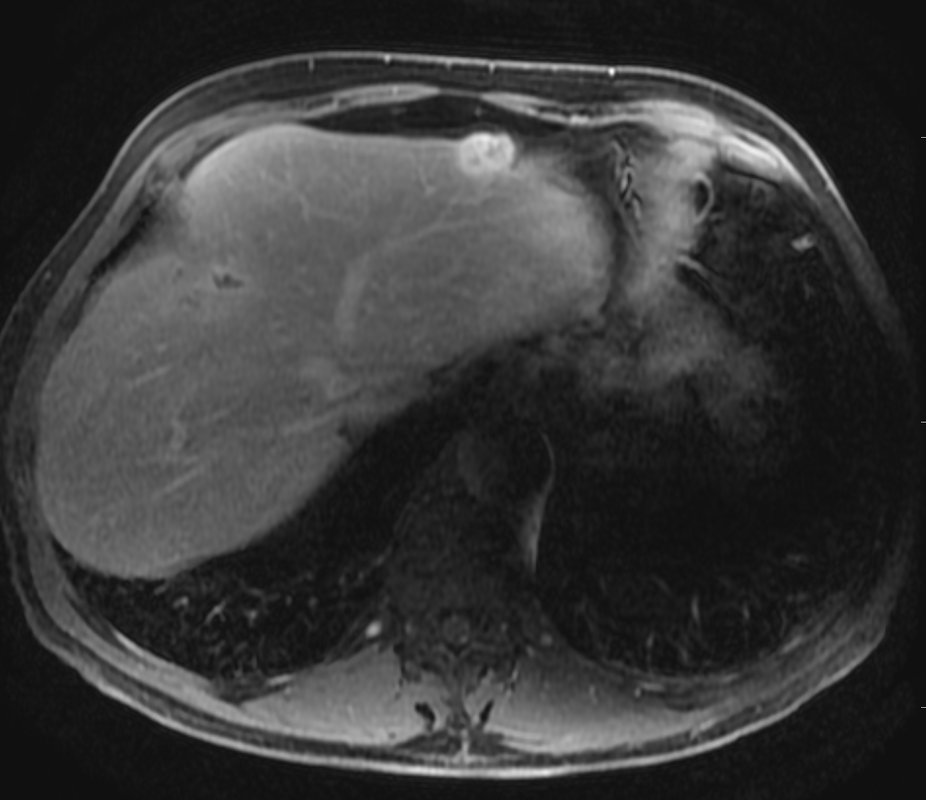
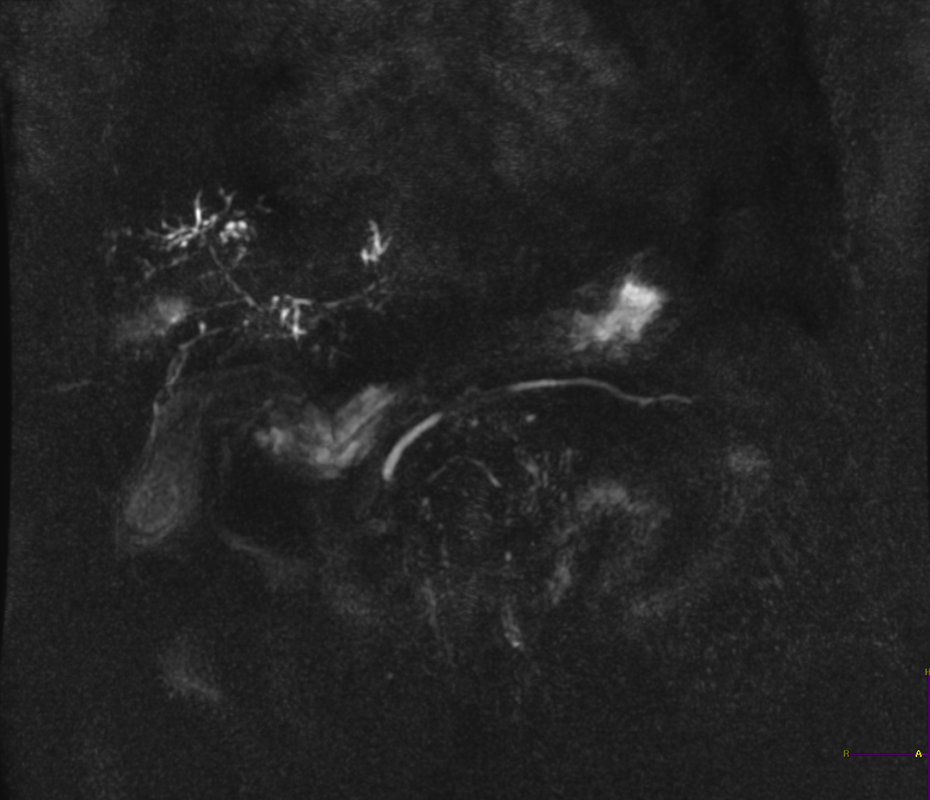
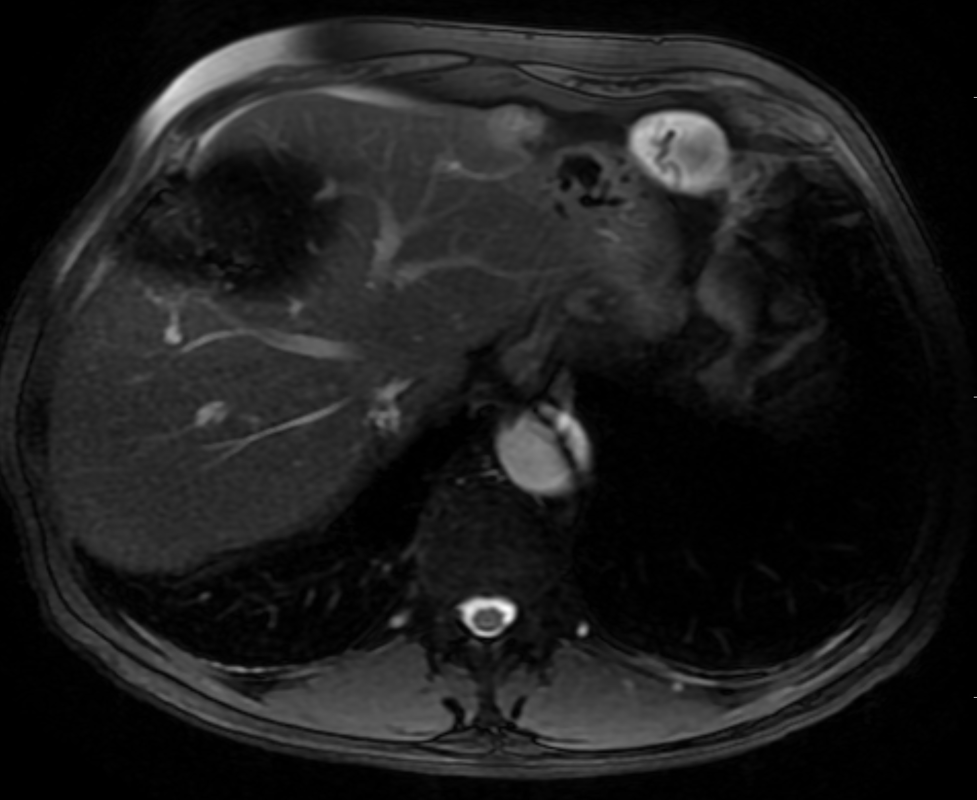
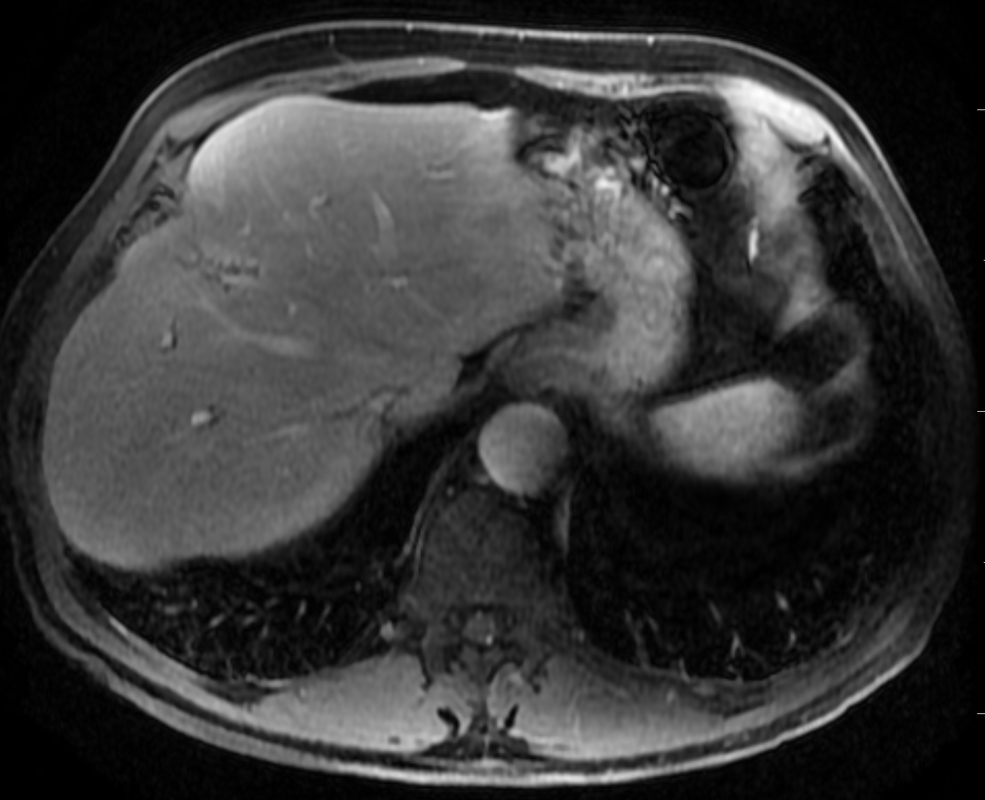
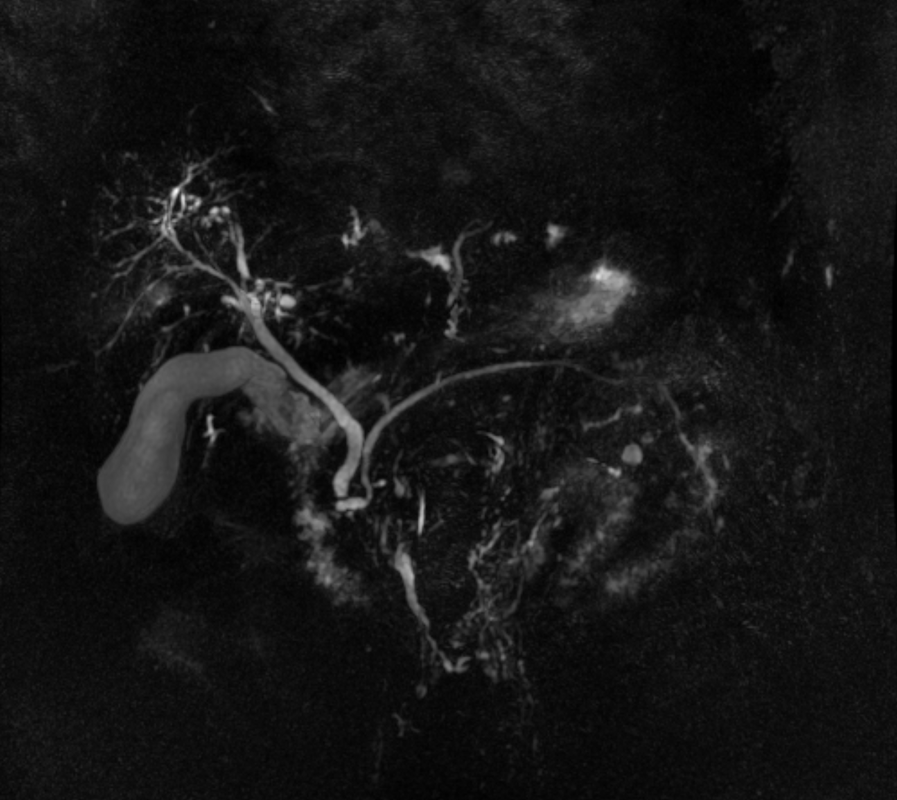
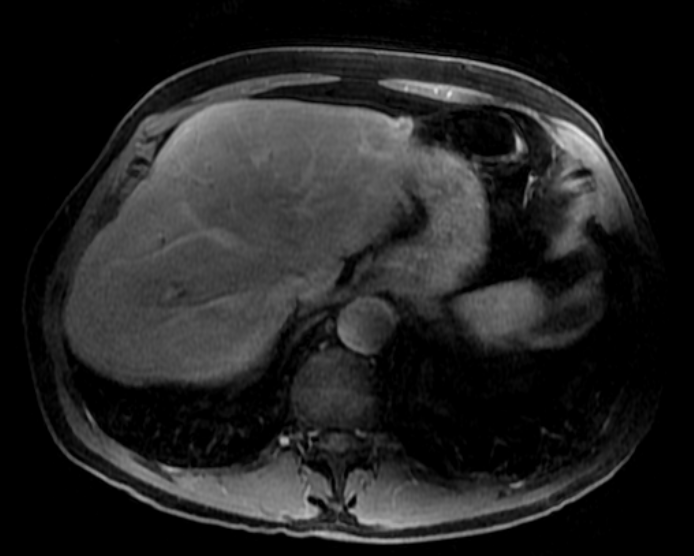
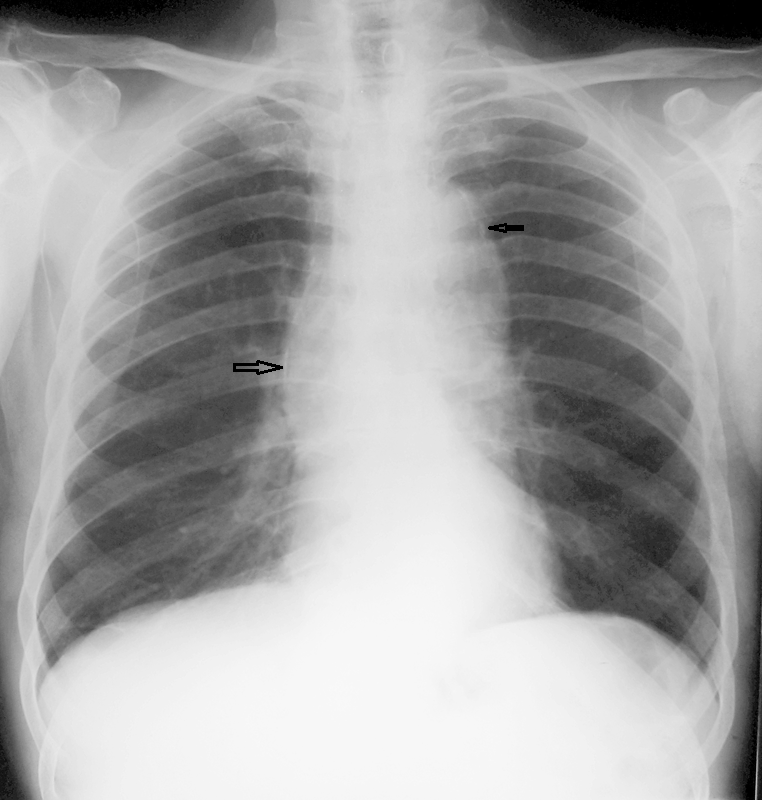
A much trickier case! The images provided from the initial Liver/MRCP examination are a T1 fat suppressed non-contrast image (top left), a FIESTA image (T2 equivalent bright blood sequence, top right), and two post contrast T1 fat suppressed images following intravenous gadolinium (second row). Thin and thick slab heavily T2 weighted MRCP images are provided on the third row. The final row demonstrates a post contrast T1 weighted fat suppressed image at 3 months. The FIESTA image has some degradation due to artefact from the lung parenchymal air affecting the right liver lobe.
The original imaging demonstrates a left liver lobe T1 hypointense and heterogenously T2 hyperintense lesion. The lesion demonstrates both peripheral enhancement but also internal extensive reticular enhancement. In addition the contrast enhanced images demonstrate that there is a tubular low T1 abnormality with peripheral enhancement in the central right liver lobe. The MRCP images demonstrate that there are normal appearances of the gallbladder, common bile duct and pancreatic duct but that the intrahepatic ducts demonstrate small clusters of focal subsegmental duct dilatation.
At 3 months, without any reported therapy the lesion has regressed to a smaller nodule of enhancement with some retraction of the liver capsule. The tubular low T1 abnormality and the associated enhancement are less conspicuous.
The appearances of the tubular abnormality in conjunction with the MRCP images indicate intrahepatic duct dilatation. However, the intrahepatic duct dilatation is discontinuous and not secondary to any obstructive stones or stricture. One could consider the possibility of primary sclerosing cholangitis, however, no typical beading is demonstrated. Additionally the dilatation demonstrates enhancement. This is a feature that indicates inflammation or possibly infection.
What about the enhancing lesion? Well the appearance of this abnormality could indicate a malignant lesion. One could then consider perhaps a case of cholangiocarcinoma with metastases, but again the non-contiguous nature of duct dilatation would not make sense and with regards to the lesion itself it is difficult to believe a malignant lesion regressed with no specific treatment.
These appearances and the regression are typical of infectious processes, in particular recurrent pyogenic cholangitis. The focal lesion is termed an inflammatory pseudotumour and often demonstrates this avid and reticular enhancement. Regression can be spontaneous or in response to antibiotics and recurrence of lesions is common. Healing can result in focal scarring as in this case.
Recurrent pyogenic cholangitis was previously referred to as oriental cholangiohepatitis and clinically is often associated with recurrent pyogenic episodes, although may be asymptomatic in the elderly. Intrahepatic marked ductal dilatation with intrahepatic duct stones can develop (hepatolithiasis). The stones are typically calcium bilirubinate. Infection of the bile with E Coli, Clonorchis sinensis or Ascaris Lumbricoides has been postulated as a cause. The condition remains more common in the far east although is not limited to that population. Long term complications include cholangiocarcinoma and intraductal papilloma formation.



 RSS Feed
RSS Feed
