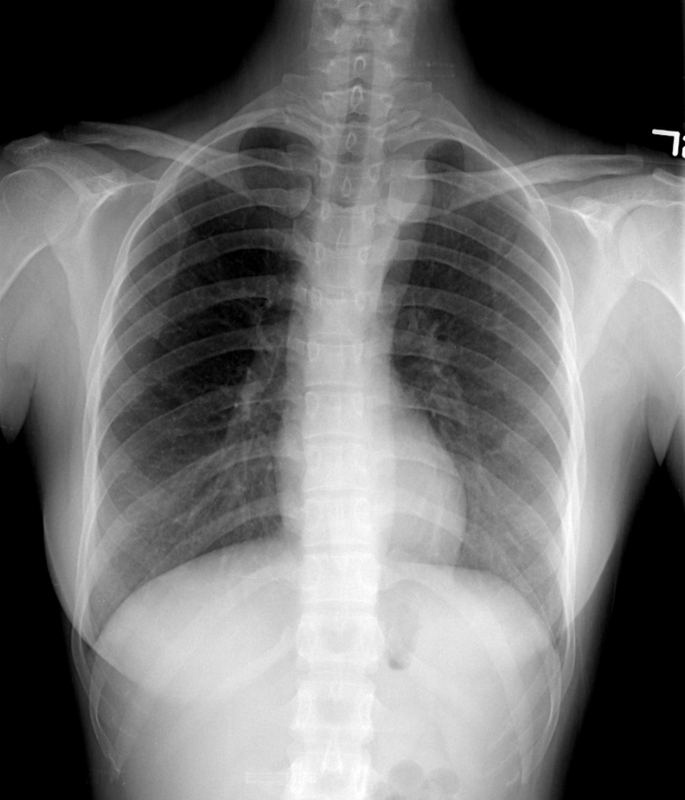
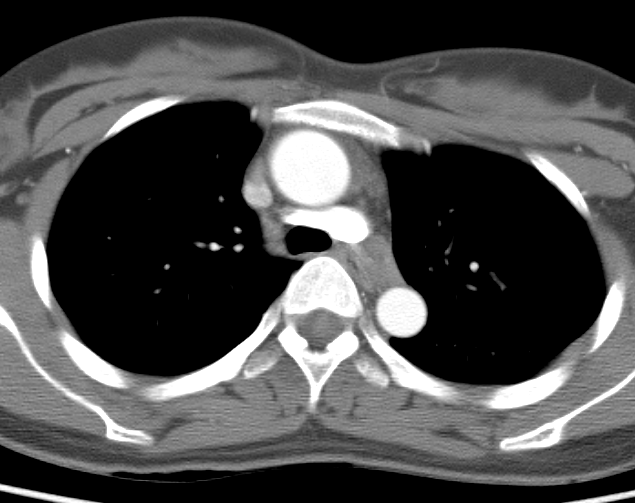
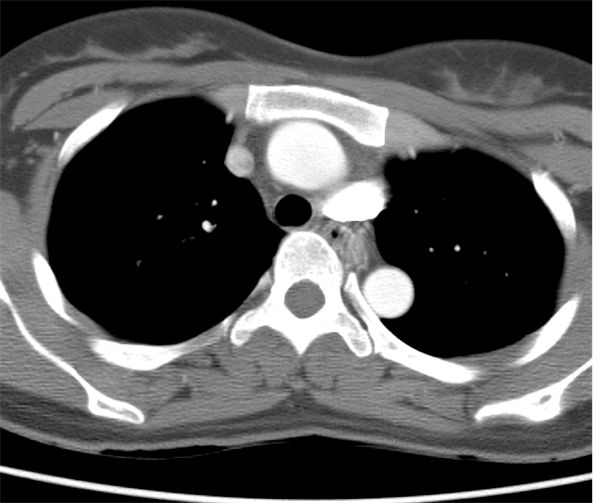
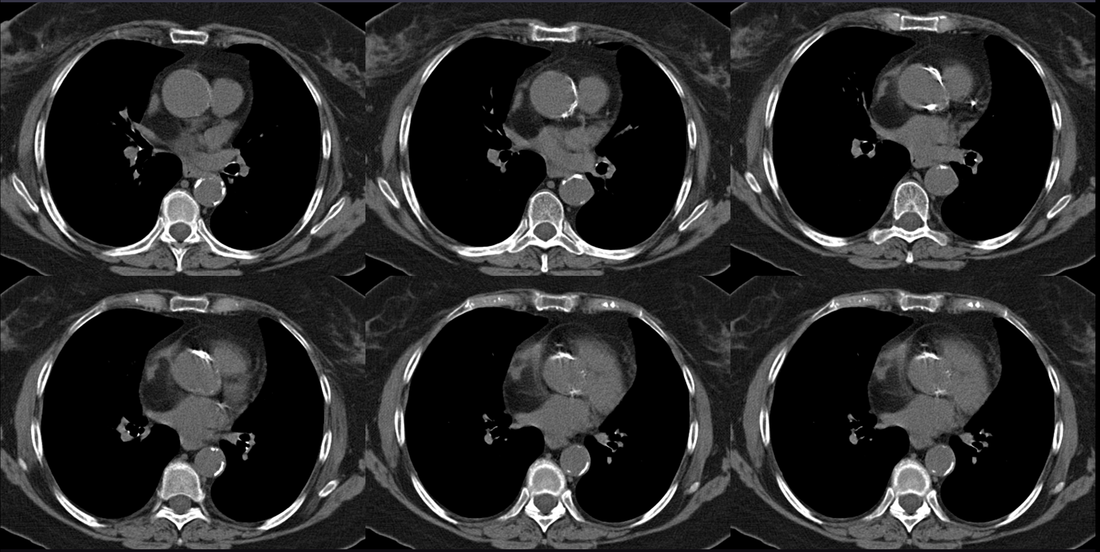
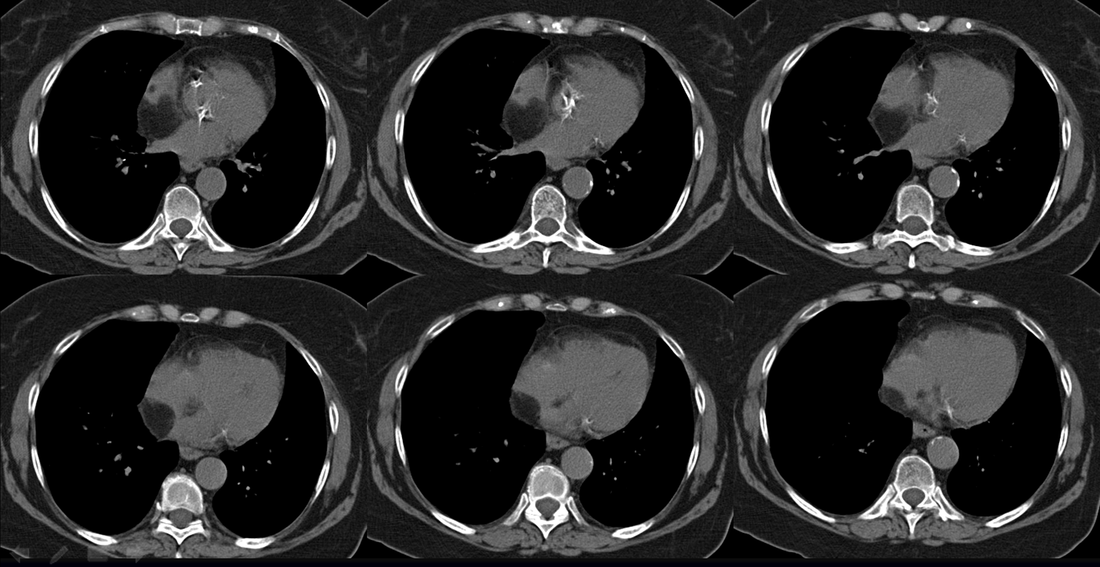
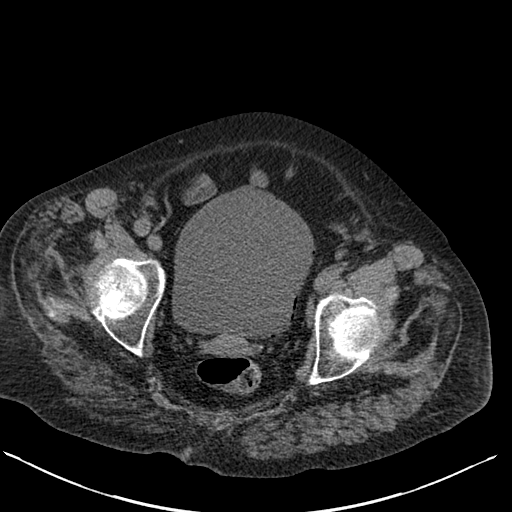
Case to Ponder 52 Answer: Lipomatous Hypertrophy of the Interatrial Septum - “Interatrial Lipoma”.27/1/2016 The CT images demonstrate a low density fatty proliferation within the interatrial septum. This has a typical dumbbell configuration, with a central stalk reflecting the fossa ovalis. This is the typical appearance of Lipomatous Hypertrophy of the Interatrial Septum (LHAS). This is sometimes referred to as an “interatrial lipoma” although it is unclear that such a distinct entity exists in this location as opposed to elsewhere in the heart and pericardium. The finding is generally an incidental finding and as in this case asymptomatic. There have been reports of possible associations with supraventricular tachycardias although it is unclear that these are not coincidental. Isolated cases of superior vena cava obstruction due to very large lesions have also been described. The incidence is unclear as the finding is under-recognised and due to limited clinical significance under-reported. An incidence of up to 1% appears more reasonable than some published estimates of 2-8%. Although there are some associations with generalised obesity these are not consistently present.
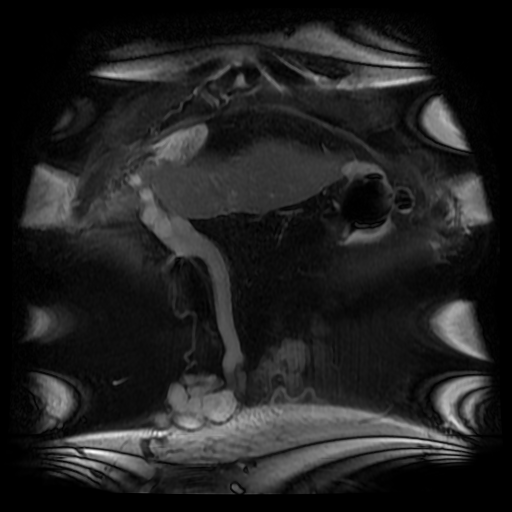
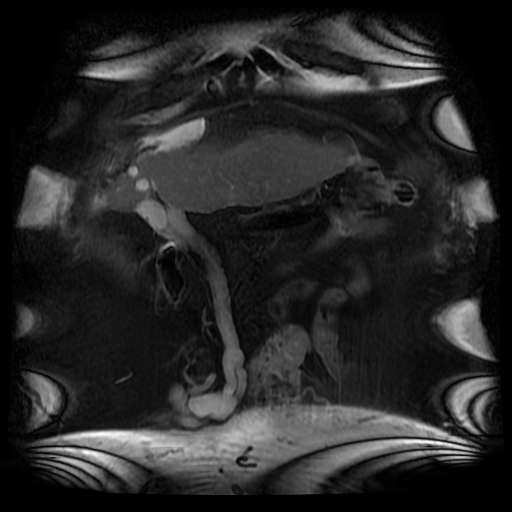
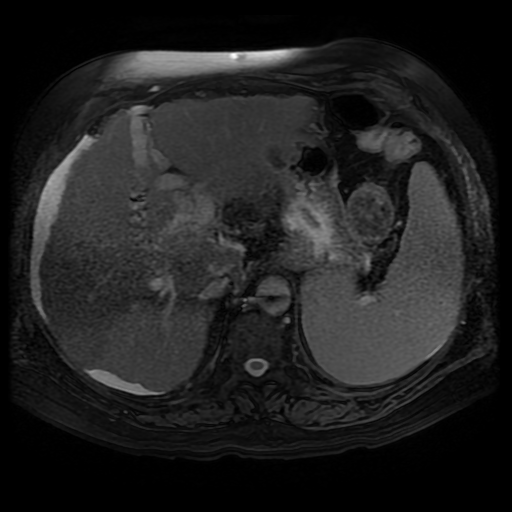
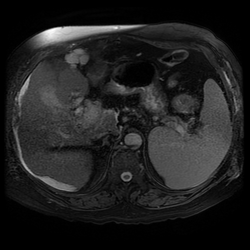
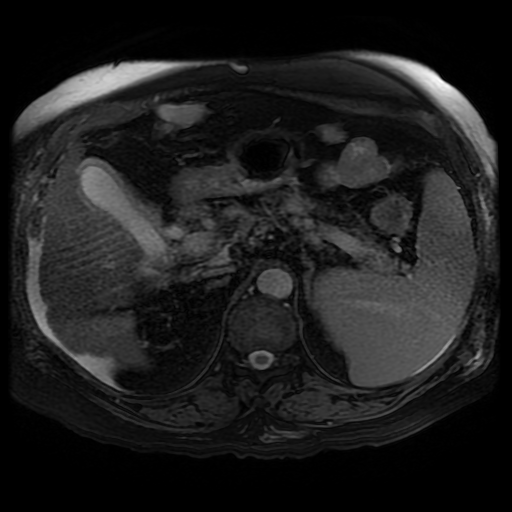
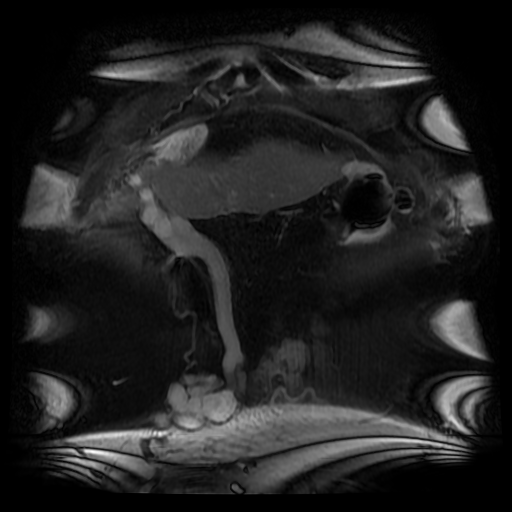
The lesion can be confused for a tumour on echocardiography for an intracardiac or atrial septal echogenic mass although the fat attenuation at CT or fat suppression on MRI images is diagnostic. In practice I find the preservation of the fossa ovalis as an anatomic landmark for determining the location of any patent foramen ovale (in acute right cardiac strain due to pulmonary embolism or pulmonary hypertension) or locating a atrial septal defect can be helpful. In my experience extension of generalised fat into the epicaridal space is demonstrated in some cases. On one occasion, I recall the interatrial lipomatous hypertrophy acting as a pathway for extension of pericardial malignant disease infiltration. This is a single non-contrast coronal image from an MRI examination (Coronal FIESTA). This is sufficient to make the clinical diagnosis, although more reference images are presented for anatomical completeness. There is a large venous structure arising from the anterior surface of the liver near the falciform ligament. This extends inferiorly into the midline where it ends in a tangle of vessels near the umbilicus. These appearances are characteristic of “Caput Medusae” the serpent head of the mythical Gorgon Medusa. These findings reflect porto-systemic circulation anastomoses developing in a patient with portal hypertension due to chronic liver disease with cirrhosis. The caput develops due to recanalization of the para-umbilical vein in the falciform ligament, a structure that usually occludes in the second week of life. As with all collateral or variceal vessels identified at CT, MRI or ultrasound it is critical to the diagnosis to consider the direction of flow and what the objective of the varices is. The object of this recanalization is to divert portal venous blood away from the high pressure liver. As the venous vessels radiate from the umbilicus they anastomose with systemic veins diverting portal venous flow. Rarely the inverse direction of flow can be seen in patients with inferior vena cava obstruction. Although recanalization of the portal vein is not uncommon a fully formed Caput medusae is an indication of severe portal hypertension. More common attempted porto-systemic anastomoses include gastro-oesophageal varices (anastomosing with the systemic lower oesophageal veins) or lienorenal shunts (splenic veins anastomosing with the left renal vein). Portosystemic shunts can also occur around the rectum due to anastomosis of the superior rectal veins (draining to the portal venous system) and inferior rectal/anal veins anastomosing to the internal iliac circulation, although these are also uncommon and seen in very advanced cases. The Caput Medusae refers to the serpent head of the Gorgon Medusa. Looking at Medusa’s directly would petrify onlookers. The image below demonstrates a Canova (1804-1806) sculpture from the Metropolitan Museum of Art in New York City. This demonstrates Perseus beheading the Gordon Medusa. In this depicted version of mythology Perseus used the invisibility cap of Hades to behead her. More commonly it is stated that Perseus slayed Medusa by viewing her reflection in a bronze shield provided by Athena. From Medusa’s blood arose Chrysaor (a golden giant) and Pegasus (the winged horse)! Radiology and Mythology on a Sunday morning!
The images demonstrate air in the lateral wall of the bladder. The location in this region indicates that the air is not free within the bladder but actually within the wall. In the absence of rare instances of trauma these appearances indicate emphysematous cystitis. This is an unusual form of urinary tract infection, characterised by gas within the bladder wall and/or bladder lumen. The presentation of patients with this condition varies from asymptomatic to severe sepsis and overall a mortality figure of 7% has been associated. An asymptomatic detection on imaging, usually CT, is common. A proportion of patients may present with pneumaturia, presumably when air is also within the bladder itself.
The typical patient is elderly and female and over 50% have diabetes, often severe. Additional risk factors include long-term catherisation and immune suppression. Associated commonest infective organisms are Escherichia coli and Klebsiella pneumonia. Most cases are treatable early in the course with antibiotics, bladder drainage, and improved diabetic glucose control. Pneumaturia or air within the bladder itself without bladder wall air may relate to other causes including prior catheterisation, fistula formation (usually colovesical due to diverticular disease or inflammatory bowel disease) or trauma. The differentiation of intraluminal air from wall air can be made by evaluating the location but also by the usually beaded non-contiguous nature of wall air compared to larger antidependent locules of intravesical air. Repositioning the patient at CT or US can be of assistance. The bilateral DP hand projection demonstrates a bilateral asymmetric arthropathy predominantly affecting the distal interphalangeal joints. There is terminal tuft resorption with a destructive pattern to the distal interphalangeal joints with loss of articulation and alignment of the distal interphalangeal joints, many of which demonstrate the typical “pencil in cup” appearance. There is tufting of the distal phalanges with minor periostitis. Overall bone density is maintained. The appearances are characteristic of psoriatic arthropathy.
Psoriatic arthropathy tends to occur in patients who already have skin manifestations of psoriasis, especially nail involvement (90%). This is a seronegative spondyloarthropathy hence patients are frequently HLA-B27 positive and usually Rheumatoid factor negative. Unlike most other arthropathies there is no sex predilection. Hand involvement is more common than feet involvement (as opposed to Reiter’s another seronegative arthritis). The hand pattern varies from a symmetric polyarthropathy, mimicking rheumatoid, to an asymmetric oligoarthropathy. Involvement of the distal interphalangeal joints typically exceeds that of the proximal interphalangeal joints or metacarpophalangeal joints. The erosive arthritis involves both the articular and juxta-articular joint margin. Resorption of the terminal phalanges is common and in combination with joint erosions this can become pronounced resulting in the “pencil-in-cup” appearance. In turn malalignment of the joint with angulation and even telescoping of phalanges often referred to as “arthritis mutilans”. Ankylosis can occur. Soft tissue swelling of an entire digit, a “sausage digit”, is also recognised. Despite the severity of disease in contradistinction to rheumatoid there is usually no osteoporosis present. Blurring of the phalanges may be seen due to periosteal reactions or whiskering at sites of tendinous insertion due to enthesopathy. These effects can be pronounced and result in “cloaking” of the phalanx, or an ivory phalanx, more typically in the foot than the hand. Apart from rheumatoid arthritis which is differentiated by distribution, and overall osteoporosis with periarticular accentuation one can also consider erosive osteoarthritis as a differential diagnosis. In erosive osteoarthritis “gull wing” central erosions are present that are differentiated from the peripheral bare erosision in psoriatic arthropathy sometimes referred to as “mouse ears”. Places still available for Mar 5-6 and Mar 21-22 2016 courses. Online interactive teaching by email starting this week. Earlier registrants see more material!
|
From Grayscale
Latest news about Grayscale Courses, Cases to Ponder and other info Categories
All
Archives
October 2018
|

|
|
Grayscale Courses est. 2015







 RSS Feed
RSS Feed
