Follow-up imaging demonstrates that there has been clearing of abnormality in the left upper zone with a tram track residual abnormality indicating bronchiectasis. At this stage the differential remains the same. Bronchial atresia is most common in the upper lobes, with some disagreement in the literature as to whether this is more common on the left or right.
On the final study we can see that there is a new ovoid opacity in the left upper zone but there is now new branching abnormality in the right upper lobe. As bronchial atresia is not bilateral, this can now be dismissed. Bronchiectasis can result in multiple areas of focal periodic mucoid impaction, but migrating impaction of large airways is the hallmark of allergic bronchopulmonary aspegillosis (ABPA). This disease is associated with a hyperimmune eosinophilic response to external antigens. The typical "finger in glove" impaction of airways is demonstrated in this case.
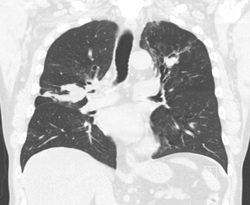
CT demonstrated below at different time points shows areas of bronchiectasis with impaction that varies with time. A feature that is considered almost pathognomonic but not present in this case is hyperdense secretions within the airways. This is postulated due to altered endobronchial metabolism and accumulation of ions of iron and manganese. Recall that although marked central varicoid bronchiectasis is typical in ABPA, that this pattern of bronchiectasis (although not usually the impaction variability) can occur in other conditions including cystic fibrosis and immunodeficiencies. Also note that ABPA is heterogenous and may be present clinically (asthma, very high IgE precipitins) but CT may demonstrate only minor bronchial wall thickening without any bronchiectasis.






 RSS Feed
RSS Feed
