In this region the possibility of a node should be considered. Nodes in this region may reflect more widespread adenopathy, however, when isolated to this left gastric/gastrohepatic ligament region careful consideration of primary malignancies of the stomach or the lower oesophagus should be assessed.
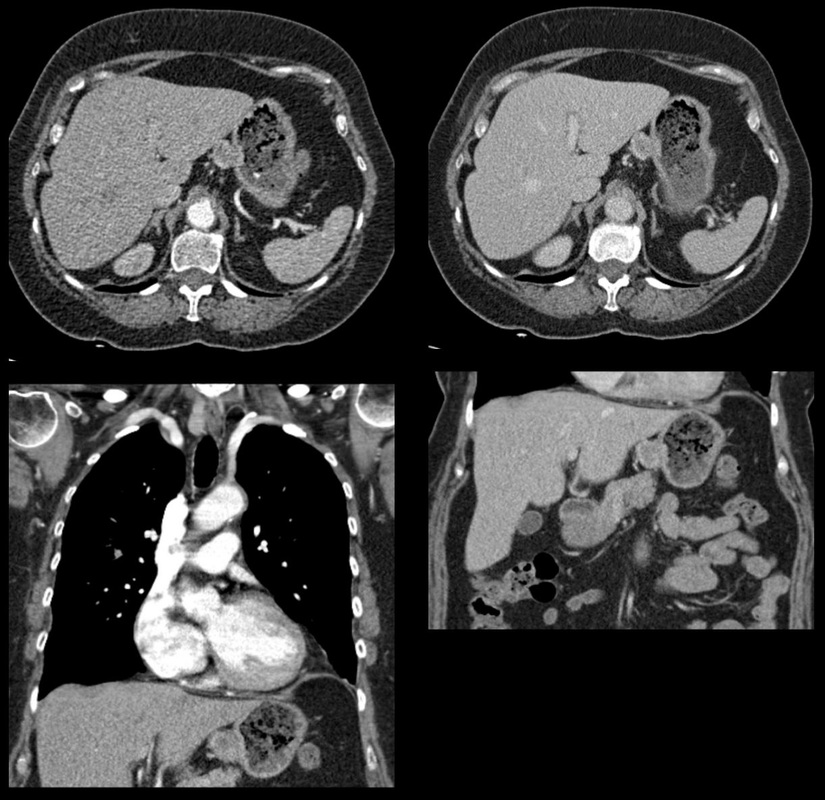
In this instance, however, the abnormality appears to arise from the gastric wall. These appearances are atypical for a gastric carcinoma that typically would present as an infiltrative or luminally narrowing lesion. The exophytic appearances in this case are typical of a gastrointestinal stromal tumour (GIST), a form of mesenchymal sarcoma, formerly known as leiomyoma or leiomyosarcoma.
GISTs are most common in the stomach (70%) and are frequently exophytic either intra or less commonly extraluminally. They can reach a large size before presentation, particularly if extraluminal but not infiltrating into other structures. Ulceration, not evident in this case, occurs in up to half of lesions. This is visible in small lesions with barium studies or at CT in larger lesions, that may contain air from luminal extension. Haemorrhage is frequently present within the lesions and with central necrosis, as in this case, lead to tumour heterogeneous density or peripheral enhancement.
GISTs are less frequently seen in other parts of the gastrointestinal tract, most commonly the small bowel, with lesser incidence in the oesophagus and elsewhere. Benign tumours of the oesophagus are still termed leiomyomas, where they are most common. GISTs can be entirely extra-enteric, termed extra-gastrointestinal occurring in the mesentery or retroperitoneum. The lesions arise from the submucosa so may be inconspicuous on endoscopy, or simply result in smooth indentation.
Presentation is typically over the age of 40, unless there is a syndromic association, such as Carney’s triad (two or three of the following: pulmonary hamartomas, gastrointestinal stromal tumours and extra-adrenal phaeochromocytoma). Presentation can be incidental such as in this case, however, if intraluminal may present with obstructive symptoms or local symptomatology if locally infiltrative to other organs or metastatic (50%). Nodal metastases are uncommon. Gastrointestinal haemorrhage is a not infrequent cause of presentation. The presentation is in many ways linked to the aggressiveness of the tumour which is highly variable. Lesions <2cm are largely considered to have a benign progression and are unlikely to recur following resection.
As distinct from genuine leiomyomas and leiomyosarcomas , GISTs contain no smooth muscle or Schwann cells. They are thought to arise from the interstitial cells of Cajal in the myenteric plexus. These cells normally express a trans-membrane receptor tyrosine kinase encoded by the KIT gene. The vast majority of GISTs exhibit activating mutations in KIT that lead to ligand-dependent KIT tyrosine kinases activation and promote tumor survival and growth. As a result treatment of irresectable GISTs has been greatly improved by the introduction of agents such as imatinib (Gleevec/Glivec) a tyrosine kinase inhibitor.
From a radiological perspective it should be noted that treatment of GIST with imatinib may not result in a reduction in size of the tumour for several months. In addition early oedema or intratumoral haemorrhage (5%) may result in an early tumour transient increase in size. In addition to PET-CT SUV activity reduction, CT imaging can demonstrate reduction in attenuation of the tumour can be seen as early as one month following treatment initiation, and perhaps as early as one week. Choi has suggested modified response criteria for GIST treatment (10% decrease in unidimensional tumor size or a 15% decrease in tumour density on contrast-enhanced CT at 8 weeks post treatment) as a better correlation to PET-CT activity reduction. Fluid overload with ascites, pleural and pericardial effusions, or subcutaneous oedema is another effect of such therapy to be aware of.
Additional Reading:
Xie Hong et al. Gastrointestinal Stromal Tumor: Role of CT in Diagnosis and in Response Evaluation and Surveillance after Treatment with Imatinib
http://pubs.rsna.org/doi/full/10.1148/rg.262055097

 RSS Feed
RSS Feed
